Biliary cystadenoma and cystadenocarcinoma CT: Difference between revisions
No edit summary |
No edit summary |
||
| Line 5: | Line 5: | ||
==CT== | ==CT== | ||
Biliary cystadenomas often are diagnosed incidentally, during imaging studies such as ultrasound or CT scan. Both abdominal ultrasound and CT scan are considered the most useful radiologic studies, allowing correct diagnosis in most cases:<ref name="RamacciatoNigri2006">{{cite journal|last1=Ramacciato|first1=Giovanni|last2=Nigri|first2=GiuseppeR|last3=D'Angelo|first3=Francesco|last4=Aurello|first4=Paolo|last5=Bellagamba|first5=Riccardo|last6=Colarossi|first6=Cristina|last7=Pilozzi|first7=Emanuela|last8=Del Gaudio|first8=Massimo|journal=World Journal of Surgical Oncology|volume=4|issue=1|year=2006|pages=76|issn=14777819|doi=10.1186/1477-7819-4-76}}</ref> | Biliary cystadenomas often are diagnosed incidentally, during imaging studies such as ultrasound or CT scan. Both abdominal ultrasound and CT scan are considered the most useful radiologic studies, allowing correct diagnosis in most cases:<ref name="RamacciatoNigri2006">{{cite journal|last1=Ramacciato|first1=Giovanni|last2=Nigri|first2=GiuseppeR|last3=D'Angelo|first3=Francesco|last4=Aurello|first4=Paolo|last5=Bellagamba|first5=Riccardo|last6=Colarossi|first6=Cristina|last7=Pilozzi|first7=Emanuela|last8=Del Gaudio|first8=Massimo|journal=World Journal of Surgical Oncology|volume=4|issue=1|year=2006|pages=76|issn=14777819|doi=10.1186/1477-7819-4-76}}</ref> | ||
*CT scan usually shows a multiloculated cyst. | *CT scan usually shows a multiloculated cyst. | ||
*Calcifications of septa or cyst wall may be observed. | *Calcifications of septa or cyst wall may be observed. | ||
*Calcifications that may be present in the septa or cyst wall are typically more apparent with CT than other imaging modalities | *Calcifications that may be present in the septa or cyst wall are typically more apparent with CT than other imaging modalities | ||
*The septa may enhance following administration of contrast. | *The septa may enhance following administration of contrast. | ||
*As is the case with ultrasound, the appearance of the cyst fluid on CT is variable depending on its composition. It can range from that of water (HU = 0) to quite hyperattenuating if the cyst has been complicated by recent hemorrhage | *As is the case with ultrasound, the appearance of the cyst fluid on CT is variable depending on its composition. It can range from that of water (HU = 0) to quite hyperattenuating if the cyst has been complicated by recent hemorrhage | ||
There are no specific imaging features that permit reliable differentiation of biliary cystadenoma from cystadenocarcinoma:<ref name=radio1>Biliary cystadenoma.Dr Yuranga Weerakkody and Radswiki et al.Radiopaedia.org 2015. http://radiopaedia.org/articles/biliary-cystadenoma</ref> | |||
There are no specific imaging features that permit reliable differentiation of biliary cystadenoma from cystadenocarcinoma | *The presence of intraluminal polypoid projections originating from the wall should raise the suspicion for cystadenocarcinoma.<ref name="RamacciatoNigri2006">{{cite journal|last1=Ramacciato|first1=Giovanni|last2=Nigri|first2=Giuseppe R|last3=D'Angelo|first3=Francesco|last4=Aurello|first4=Paolo|last5=Bellagamba|first5=Riccardo|last6=Colarossi|first6=Cristina|last7=Pilozzi|first7=Emanuela|last8=Del Gaudio|first8=Massimo|journal=World Journal of Surgical Oncology|volume=4|issue=1|year=2006|pages=76|issn=14777819|doi=10.1186/1477-7819-4-76}}</ref> | ||
*The presence of intraluminal polypoid projections originating from the wall should raise the suspicion for cystadenocarcinoma. | |||
*Hypervascularity of mural nodules on CT also suggests malignancy.<ref name="Ahanatha PillaiVelayutham2012">{{cite journal|last1=Ahanatha Pillai|first1=Sastha|last2=Velayutham|first2=Vimalraj|last3=Perumal|first3=Senthilkumar|last4=Ulagendra Perumal|first4=Srinivasan|last5=Lakshmanan|first5=Anand|last6=Ramaswami|first6=Sukumar|last7=Ramasamy|first7=Ravi|last8=Sathyanesan|first8=Jeswanth|last9=Palaniappan|first9=Ravichandran|last10=Rajagopal|first10=Surendran|title=Biliary Cystadenomas: A Case for Complete Resection|journal=HPB Surgery|volume=2012|year=2012|pages=1–6|issn=0894-8569|doi=10.1155/2012/501705}}</ref> | *Hypervascularity of mural nodules on CT also suggests malignancy.<ref name="Ahanatha PillaiVelayutham2012">{{cite journal|last1=Ahanatha Pillai|first1=Sastha|last2=Velayutham|first2=Vimalraj|last3=Perumal|first3=Senthilkumar|last4=Ulagendra Perumal|first4=Srinivasan|last5=Lakshmanan|first5=Anand|last6=Ramaswami|first6=Sukumar|last7=Ramasamy|first7=Ravi|last8=Sathyanesan|first8=Jeswanth|last9=Palaniappan|first9=Ravichandran|last10=Rajagopal|first10=Surendran|title=Biliary Cystadenomas: A Case for Complete Resection|journal=HPB Surgery|volume=2012|year=2012|pages=1–6|issn=0894-8569|doi=10.1155/2012/501705}}</ref> | ||
| Line 32: | Line 25: | ||
</gallery> | </gallery> | ||
Magnetic resonance imaging (MRI) can provide additional informations on the nature of the cystic fluid (i.e., serous vs. mucinous vs. hemorrhagic). Endoscopic retrograde cholangiopancreatography (ERCP), even if rarely employed, may show a cystic cavity communicating with the biliary tree.<ref name="RamacciatoNigri2006">{{cite journal|last1=Ramacciato|first1=Giovanni|last2=Nigri|first2=Giuseppe R|last3=D'Angelo|first3=Francesco|last4=Aurello|first4=Paolo|last5=Bellagamba|first5=Riccardo|last6=Colarossi|first6=Cristina|last7=Pilozzi|first7=Emanuela|last8=Del Gaudio|first8=Massimo|journal=World Journal of Surgical Oncology|volume=4|issue=1|year=2006|pages=76|issn=14777819|doi=10.1186/1477-7819-4-76}}</ref> | |||
==References== | ==References== | ||
{{Reflist|2}} | {{Reflist|2}} | ||
Revision as of 20:51, 17 November 2015
|
Biliary cystadenoma and cystadenocarcinoma Microchapters |
|
Differentiating Biliary cystadenoma and cystadenocarcinoma from other Diseases |
|---|
|
Diagnosis |
|
Treatment |
|
Case Studies |
|
Biliary cystadenoma and cystadenocarcinoma CT On the Web |
|
American Roentgen Ray Society Images of Biliary cystadenoma and cystadenocarcinoma CT |
|
Directions to Hospitals Treating Biliary cystadenoma and cystadenocarcinoma |
|
Risk calculators and risk factors for Biliary cystadenoma and cystadenocarcinoma CT |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]
Overview
CT
Biliary cystadenomas often are diagnosed incidentally, during imaging studies such as ultrasound or CT scan. Both abdominal ultrasound and CT scan are considered the most useful radiologic studies, allowing correct diagnosis in most cases:[1]
- CT scan usually shows a multiloculated cyst.
- Calcifications of septa or cyst wall may be observed.
- Calcifications that may be present in the septa or cyst wall are typically more apparent with CT than other imaging modalities
- The septa may enhance following administration of contrast.
- As is the case with ultrasound, the appearance of the cyst fluid on CT is variable depending on its composition. It can range from that of water (HU = 0) to quite hyperattenuating if the cyst has been complicated by recent hemorrhage
There are no specific imaging features that permit reliable differentiation of biliary cystadenoma from cystadenocarcinoma:[2]
- The presence of intraluminal polypoid projections originating from the wall should raise the suspicion for cystadenocarcinoma.[1]
- Hypervascularity of mural nodules on CT also suggests malignancy.[3]
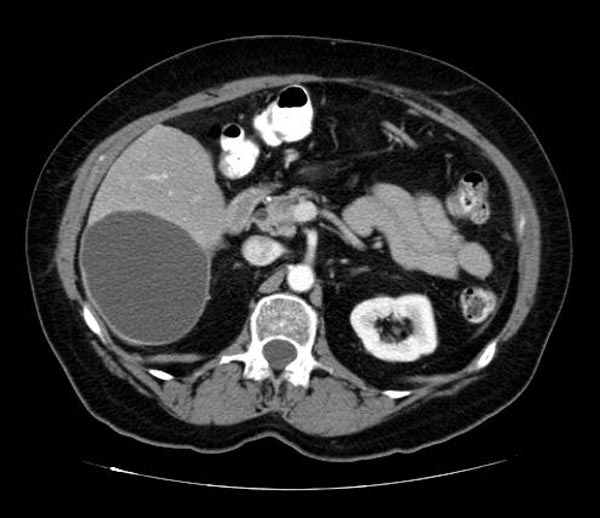
(Images courtesy of RadsWiki)
-
CT image demonstates a biliary cystadenoma
-
CT image demonstates a biliary cystadenoma
Magnetic resonance imaging (MRI) can provide additional informations on the nature of the cystic fluid (i.e., serous vs. mucinous vs. hemorrhagic). Endoscopic retrograde cholangiopancreatography (ERCP), even if rarely employed, may show a cystic cavity communicating with the biliary tree.[1]
References
- ↑ 1.0 1.1 1.2 Ramacciato, Giovanni; Nigri, GiuseppeR; D'Angelo, Francesco; Aurello, Paolo; Bellagamba, Riccardo; Colarossi, Cristina; Pilozzi, Emanuela; Del Gaudio, Massimo (2006). World Journal of Surgical Oncology. 4 (1): 76. doi:10.1186/1477-7819-4-76. ISSN 1477-7819. Missing or empty
|title=(help) - ↑ Biliary cystadenoma.Dr Yuranga Weerakkody and Radswiki et al.Radiopaedia.org 2015. http://radiopaedia.org/articles/biliary-cystadenoma
- ↑ Ahanatha Pillai, Sastha; Velayutham, Vimalraj; Perumal, Senthilkumar; Ulagendra Perumal, Srinivasan; Lakshmanan, Anand; Ramaswami, Sukumar; Ramasamy, Ravi; Sathyanesan, Jeswanth; Palaniappan, Ravichandran; Rajagopal, Surendran (2012). "Biliary Cystadenomas: A Case for Complete Resection". HPB Surgery. 2012: 1–6. doi:10.1155/2012/501705. ISSN 0894-8569.