Autoimmune pancreatitis: Difference between revisions
Iqra Qamar (talk | contribs) |
Feham Tariq (talk | contribs) No edit summary |
||
| (10 intermediate revisions by 2 users not shown) | |||
| Line 6: | Line 6: | ||
}} | }} | ||
{{Autoimmune pancreatitis}} | {{Autoimmune pancreatitis}} | ||
{{CMG}}, {{AE}}:{{IQ}} | {{CMG}}, {{AE}}:{{IQ}}{{FT}} | ||
{{SK}} Primary inflammatory pancreatitis, | {{SK}} Primary inflammatory pancreatitis, Lymphoplasmacytic sclerosing pancreatitis, Pseudotumorous pancreatitis, Chronic pancreatitis with irregular narrowing of the main pancreatic duct, Nonalcoholic duct destructive chronic pancreatitis. | ||
== | ==[[Autoimmune pancreatitis overview|Overview]]== | ||
== | ==[[Autoimmune pancreatitis historical perspective|Historical Perspective]]== | ||
== | ==[[Autoimmune pancreatitis classification|Classification]]== | ||
== | ==[[Autoimmune pancreatitis pathophysiology|Pathophysiology]]== | ||
== | ==[[Autoimmune pancreatitis causes|Causes]]== | ||
== | ==[[Autoimmune pancreatitis differential diagnosis|Differentiating Sheehan's syndrome from other Diseases]]== | ||
== | ==[[Autoimmune pancreatitis epidemiology and demographics|Epidemiology and Demographics]]== | ||
==Natural History, Complications and Prognosis== | ==[[Autoimmune pancreatitis risk factors|Risk Factors]]== | ||
==[[Autoimmune pancreatitis screening|Screening]]== | |||
==[[Autoimmune pancreatitis natural history, complications and prognosis|Natural History, Complications and Prognosis]]== | |||
==Diagnosis== | ==Diagnosis== | ||
[[Autoimmune pancreatitis diagnostic study of choice|Diagnostic Study of Choice]] | [[Autoimmune pancreatitis history and symptoms|History and Symptoms]] | [[Autoimmune pancreatitis physical examination|Physical Examination]] | [[Autoimmune pancreatitis laboratory findings|Laboratory Findings]] | [[Autoimmune pancreatitis x ray|X Ray]] | [[Autoimmune pancreatitis CT scan|CT]] | [[Autoimmune pancreatitis MRI|MRI]] | [[Autoimmune pancreatitis echocardiography and ultrasound|Echocardiography and Ultrasound]] | [[Autoimmune pancreatitis other imaging findings|Other Imaging Findings]] | [[Autoimmune pancreatitis other diagnostic studies|Other Diagnostic Studies]] | |||
[[ | |||
==Treatment== | |||
== | |||
[[Autoimmune pancreatitis medical therapy|Medical Therapy]] | [[Autoimmune pancreatitis surgery|Surgery]] | [[Autoimmune pancreatitis primary prevention|Primary Prevention]] | [[Autoimmune pancreatitis secondary prevention|Secondary Prevention]] | | |||
==References== | ==References== | ||
Latest revision as of 16:18, 31 July 2018
| Autoimmune pancreatitis | |
 | |
|---|---|
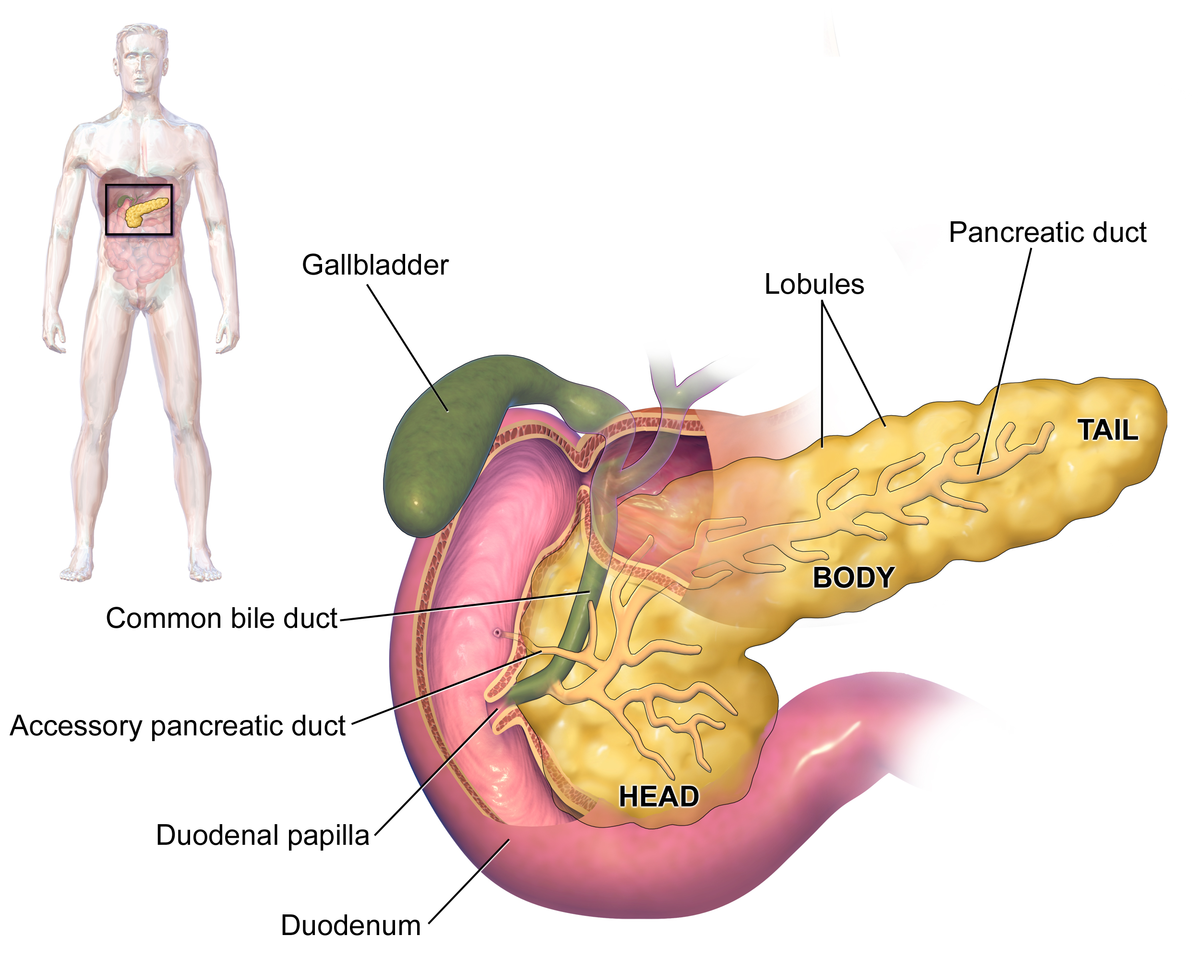
| Pancreas[1] |
|
Autoimmune pancreatitis Microchapters |
|
Diagnosis |
|---|
|
Treatment |
|
Case Studies |
|
Autoimmune pancreatitis On the Web |
|
American Roentgen Ray Society Images of Autoimmune pancreatitis |
|
Risk calculators and risk factors for Autoimmune pancreatitis |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1], Associate Editor(s)-in-Chief: :Iqra Qamar M.D.[2]Feham Tariq, MD [3]
Synonyms and keywords: Primary inflammatory pancreatitis, Lymphoplasmacytic sclerosing pancreatitis, Pseudotumorous pancreatitis, Chronic pancreatitis with irregular narrowing of the main pancreatic duct, Nonalcoholic duct destructive chronic pancreatitis.
Overview
Historical Perspective
Classification
Pathophysiology
Causes
Differentiating Sheehan's syndrome from other Diseases
Epidemiology and Demographics
Risk Factors
Screening
Natural History, Complications and Prognosis
Diagnosis
Diagnostic Study of Choice | History and Symptoms | Physical Examination | Laboratory Findings | X Ray | CT | MRI | Echocardiography and Ultrasound | Other Imaging Findings | Other Diagnostic Studies
Treatment
Medical Therapy | Surgery | Primary Prevention | Secondary Prevention |