Aortic aneurysm: Difference between revisions
Jose Loyola (talk | contribs) |
Jose Loyola (talk | contribs) |
||
| Line 181: | Line 181: | ||
The aneurysms tend to grow slowly and most of them will never rupture. As they grow, however, their symptoms become more evident and present with mass effects over surrounding structures and pain. They may present with thoracic symptoms: interscapular or central pain, ripping chest pain and dyspnea. Atypical presentations include hoarseness, dizziness and dysphagia, due to esophageal compression.<ref>Hiller, H. G., and N. R. F. Lagattolla. "Thoracic aortic aneurysm presenting with dysphagia: a fatal delay in diagnosis." ''Thoracic surgical science'' 4 (2007).</ref> Aneurysm rupture lead to massive internal bleeding, hypovolemic shock and it is usually fatal. | The aneurysms tend to grow slowly and most of them will never rupture. As they grow, however, their symptoms become more evident and present with mass effects over surrounding structures and pain. They may present with thoracic symptoms: interscapular or central pain, ripping chest pain and dyspnea. Atypical presentations include hoarseness, dizziness and dysphagia, due to esophageal compression.<ref>Hiller, H. G., and N. R. F. Lagattolla. "Thoracic aortic aneurysm presenting with dysphagia: a fatal delay in diagnosis." ''Thoracic surgical science'' 4 (2007).</ref> Aneurysm rupture lead to massive internal bleeding, hypovolemic shock and it is usually fatal. | ||
'''Abdominal aortic aneurysms:''' as the thoracic aneurysms, they begin asymptomatic but may cause symptoms as they grow and compress surrounding structures.<ref name=":2">Abdominal Aortic Aneurysm (AAA) Symptoms - Stanford Healthcare | '''Abdominal aortic aneurysms:''' as the thoracic aneurysms, they begin asymptomatic but may cause symptoms as they grow and compress surrounding structures.<ref name=":2">Abdominal Aortic Aneurysm (AAA) Symptoms - Stanford Healthcare | ||
Revision as of 18:10, 2 June 2020
| Resident Survival Guide |
| Aortic aneurysm | |
 | |
|---|---|
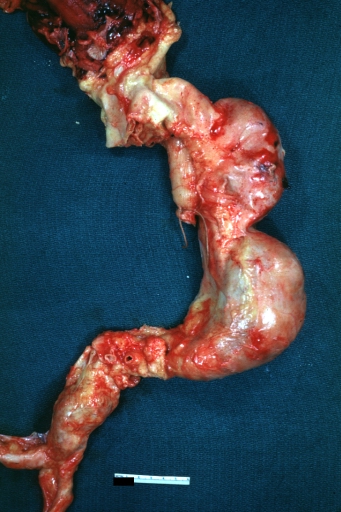
| Atherosclerotic Aneurysm: Gross, an excellent example, natural color, external view of typical thoracic aortic aneurysms Image courtesy of Professor Peter Anderson DVM PhD and published with permission © PEIR, University of Alabama at Birmingham, Department of Pathology |
|
WikiDoc Resources for Aortic aneurysm |
|
Articles |
|---|
|
Most recent articles on Aortic aneurysm Most cited articles on Aortic aneurysm |
|
Media |
|
Powerpoint slides on Aortic aneurysm |
|
Evidence Based Medicine |
|
Clinical Trials |
|
Ongoing Trials on Aortic aneurysm at Clinical Trials.gov Trial results on Aortic aneurysm Clinical Trials on Aortic aneurysm at Google
|
|
Guidelines / Policies / Govt |
|
US National Guidelines Clearinghouse on Aortic aneurysm NICE Guidance on Aortic aneurysm
|
|
Books |
|
News |
|
Commentary |
|
Definitions |
|
Patient Resources / Community |
|
Patient resources on Aortic aneurysm Discussion groups on Aortic aneurysm Patient Handouts on Aortic aneurysm Directions to Hospitals Treating Aortic aneurysm Risk calculators and risk factors for Aortic aneurysm
|
|
Healthcare Provider Resources |
|
Causes & Risk Factors for Aortic aneurysm |
|
Continuing Medical Education (CME) |
|
International |
|
|
|
Business |
|
Experimental / Informatics |
For patient information on Thoracic aortic aneurysm, click here
For patient information on Abdominal aortic aneurysm, click here
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1], Associate Editor(s)-in-Chief: Lina Ya'qoub, MD Associate Editor-In-Chief: Cafer Zorkun, M.D., Ph.D. [2]
Overview
An aortic aneurysm is a dilation of the aorta in which the aortic diameter is ≥ 3.0 cm[1], usually representing an underlying weakness in the wall of the aorta at that location. While the stretched vessel may occasionally cause discomfort, a greater concern is the risk of rupture which causes severe pain, massive internal hemorrhage which are often fatal. Aneurysms often are a source of blood clots (emboli) stemming from the most common etiology of atherosclerosis.
Classification
There are 2 types of aortic aneurysms: thoracic and abdominal. These can be further classified according to the respective part of the vessel that's been affected:
- Thoracic aortic aneurysm, which occur in the thoracic aorta (runs through the chest);
- Abdominal aortic aneurysm, which occur in the abdominal aorta, are the most common.
- Suprarenal - not as common, often more difficult to repair surgically due to the presence of many aortic branches;
- Infrarenal - often more easily surgically repaired and more common;
- Pararenal - aortic aneurysm is infrarenal but affects renal arteries;
- Juxtarenal - infrarenal aortic aneurysm that affects the aorta just below the renal arteries.
Thoracoabdominal aortic aneurysm may also be classified according to Crawford classification into 5 subtypes/groups:
- Type 1: from the origin of left subclavian artery in descending thoracic aorta to the supra-renal abdominal aorta.
- Type 2: from the left subclavian to the aorto-iliac bifurcation.
- Type 3: from distal thoracic aorta to the aorto-iliac bifurcation
- Type 4: limited to abdominal aorta below the diaphragm
- Type 5: from distal thoracic aorta to celiac and superior mesenteric origins, but not the renal arteries.[2]
Historical Perspective
Aortic aneurysm was first recorded by Antyllus, a Greek surgeon, in the second century AD. In the Renaissaince era, in 1555, Vesalius first diagnosed an abdominal aortic aneurysm. The first publication on the pathology with case studies was published by Lancisi in 1728. Finally, in 1817, Astley Cooper was the first surgeon to ligate the abdominal aorta to treat a ruptured iliac aneurysm. In 1888, Rudoff Matas came up with the concept of endoaneurysmorrhaphy. [3]
Pathophysiology
The aortic aneurysms are a multifactorial disease associated with genetic and environmental risk factors. Marfan's syndrome and Ehlers-Danlos syndrome are associated with the disease, but there are also rarer syndromes like the Loeys-Dietz syndrome that are associated as well. Even in patients that do not have genetic syndromes, it has been observed that genetics can also play a role on aortic aneurysms' development. There has been evidence of genetic heterogeneity as there has already been documented in intracranial aneurysms.[4] The genetic alterations associated with these genetic syndromes are the following:
| Disease | Involved Cellular Pathway | Mutated Gene(s) | Affected Protein(s) |
|---|---|---|---|
| Ehlers-Danlos syndrome type IV | Extracellular Matrix Proteins | COL3A1 | Collagen type III |
| Marfan's syndrome | Extracellular Matrix Proteins | FBN1 | Fibrillin-1 |
| Loeys-Dietz syndrome | TGF-β Pathway | TGFBR1/TGFBR2 | |
| Aneurysm-Osteoarthritis Syndrome | SMAD3 | SMAD3 | |
| Autosomal Dominant Polycystic Kidney Disease | Ciliopathy | PKD1PKD2 | Polycystin 1
Polycystin 2 |
| Turner Syndrome | Meiotic Error with Monosomy, Mosaicism, or De Novo Germ Cell Mutation | 45X
45XO |
Partial or Complete Absence of X Chromosome |
| Bicuspid Aortic Valve with TAA | Neural Crest Migration | NOTCH1 | Notch 1 |
| Familial TAA | Smooth Muscle Contraction Proteins | ACTA2 | α-Smooth Muscle Actin |
| Familial TAA with Patent Ductus Arteriosus | Smooth Muscle Contraction Proteins | MYH11 | Smooth Muscle Myosin |
| Familial TAA | Smooth Muscle Contraction Proteins | MYLK | Myosin Light Chain Kinase |
| Familial TAA | Smooth Muscle Contraction Proteins | PRKG1 | Protein Kinase c-GMP Dependent, type I |
| Loeys-Dietz Syndrome variants | TGF-β Pathway | TGF-βR1TGF-βR2SMAD3TGF-β2TGF-β3 |
These genetic diseases mostly affect either the synthesis of extracellular matrix protein or damage the smooth muscle cells both important component's of the aortic wall. Injury to any of these components lead to weakening of the aortic wall and dilation - resulting in aneurysm formation.
The aorta is the largest vessel of the body, but it is not homogenous. Its upper segment is composed by a larger proportion of elastin in comparison to collagen, therefore being more distensible. The lower segment has a larger proportion of collagen, therefore it is less distensible. It is also where most of the atherosclerotic plaques of the aorta are located.[1] Historically it was thought that abdominal and thoracic aortic aneurysms were caused by the same etiology: atherosclerotic degeneration of the aortic wall, but recently it has been theorized that they are indeed different diseases.[1]
The aortic arch mostly derives from the neural crest cell which differentiate into smooth muscle cells. These smooth muscle cells are probably more adapted to remodel the thoracic aorta and manage the higher pulse pressure and ejection volume due to increased production of elastic lamellae during development and growth.[1] The abdominal aorta remains with cells of mesodermal origin, which are more similar to that of the original primitive arterial. That difference results in the neural crest cell precursors of the thoracic aorta being able to respond differently to various cytokines and growth factors than the mesodermal precursors of the abdominal aorta,[6] such as homocysteine[7] and angiotensin II.[8]
When neural crest vascular smooth muscle cells are treated with TGF-β they demonstrate increased collagen production, while mesodermal vascular smooth muscle cell did not.[9] Not coincidently, mutations of the TGF-β receptor can cause thoracic aortic aneurysm but do not cause abdominal aortic ones.
The thoracic and abdominal aorta are very structurally different. While they both have three layers: intimal, medial and adventitia, the media of the thoracic aorta is comprised of approximately 60 units divided into vascular and avascular regions. The abdominal aorta consists of about 30 units and is entirely avascular - being dependent on trans-intimal diffusion of nutrients for its smooth muscle cells to survive.[10] It is believed that both differences explain why the abdominal aorta is more likely to form aneurysms.
The development of aortic aneurysms is defined by: inflammation: infiltration of the vessel wall by lymphocytes and macrophage; extracellular matrix damage: destruction of elastin and collagen by proteases (also metalloproteinases) in the media and adventitia; cellular damage: loss of smooth muscle cells with thinning of the media; and insufficient repair: neovascularization.[11]
In summary:
- The pathogenesis of aortic aneurysm is characterized by progressive dilation, rupture, and may present with dissection;
- The pathological processes that lead to abdominal and thoracic aortic aneurysms may be very different from one another;
- The fibrillin-1 gene mutation has been associated with the development of thoracic aortic aneurysms in Marfan's syndrome;
- Other gene mutations coding for collagen, elastin and other elements of the extracellular matrix have been associated with the development of aneurysms in some genetic disorders, including Ehlers-Danlos syndrome and others;
- Mutations in the TGF-β pathway have also been described in the pathogenesis of aortic aneurysms in multiple genetic disorders, including Loeys-Dietz syndrome.
Clinical Features
Differentiating Aortic Aneurysm from other Diseases
Thoracic aortic aneurysms: differential diagnosis include other causes of chest pain: acute aortic dissection, acute pericarditis, aortic regurgitation, heart failure, hypertensive emergencies, infective endocarditis, myocardial Infarction, pulmonary embolism, superior vena cava syndrome. [12]
Abdominal aortic aneurysms: differential diagnosis include causes of pulsatile abdominal mass and/or abdominal pain such as ruptured viscus, strangulated hernia, ruptured visceral artery aneurysms, mesenteric ischemia, acute cholecystitis, ruptured hepatobiliary cancer, acute pancreatitis, lymphomas, and diverticular abscess.[13]
These conditions can be easily differentiated using abdominal or thoracic imaging.
Epidemiology and Demographics
In the United States alone 15,000 people die yearly due to aortic aneurysms and it is the 13th leading cause of death. 1-2% of the population may have aortic aneurysms and prevalence rises up to 10% in older age groups. The disease varies according to where it takes place. In the thorax, the aortic arch is the less affected segment (10%) and the most common is the ascending aorta (50%). Regarding abdominal aneurysms, the infrarenal segment aortic aneurysms are three times more prevalent than the aortic aneurysms and dissections.[4]
Regarding other factors as age, abdominal aortic aneurysms usually present 10 years later than thoracic aortic aneurysms. Both lesions are more present in men, but the proportion is much higher regarding abdominal aortic aneurysms (6:1 male:female ratio) in comparison to thoracic ones.[4]
Abdominal aortic aneurysms also affect patients differently regarding race, as they are more prevalent among whites than blacks, asians and hispanics. It also seems to be declining in prevalence as evidenced by a Swedish study that found out a 2% prevalence of abdominal aortic aneurysms in comparison to earlier studies which reported 4-8%, probably due to risk-factor modification. [14]
Risk Factors
Many risk factors are common between both forms of aortic aneurysms, but some are specific for each presentation:
- Abdominal aortic aneurysm: smoking, male gender, age (>65 years), race (white), family history, other aneurysms.[13]
- Thoracic aortic aneurysm: smoking, age (>65 years), hypertension, atherosclerosis, family history, Marfan's syndrome, bicuspid aortic valve. [15]
Natural History, Complications and Prognosis
- The majority of patients with aortic aneurysms remain asymptomatic for years.
- Early clinical features include abdominal pain, pulsatile abdominal mass, and chest pain.
- If left untreated, patients with progressively enlarging AAA, >0.5cm increase in size over 6 months or AAA of >5.5cm in diameter, are at increased risk of aneurysm rupture and death.
- Common complications of AAA include rupture, dissection, systemic embolization and death.
- Prognosis is generally good if screened and managed appropriately, and the 5-year survival rate of patients with repaired AAA is approximately 73%.
Diagnosis
Diagnostic Criteria
- The diagnosis of AAA is made when at least [number] of the following diagnostic criteria are met:
- Dilation of vessel diameter >50% its normal diameter
- Full thickness dilation: involving all three layers of the vessel
Symptoms:
Aortic aneurysms are largely an asymptomatic condition, but symptoms present differently according to the affected segment of the aorta.
Thoracic aortic aneurysms: patients are usually diagnosed in these contexts:
- Incidental finding as part of a routine examination (transthoracic echocardiography, computerized tomography of the chest, cardiac magnetic resonance imaging, routine chest radiograph);
- Acute presentation with thoracic aortic dissection or aneurysm rupture;
- Screening due to a relative of a patient presenting with aortic disease;
- Part of a known congenital cardiac condition. [16]
The aneurysms tend to grow slowly and most of them will never rupture. As they grow, however, their symptoms become more evident and present with mass effects over surrounding structures and pain. They may present with thoracic symptoms: interscapular or central pain, ripping chest pain and dyspnea. Atypical presentations include hoarseness, dizziness and dysphagia, due to esophageal compression.[17] Aneurysm rupture lead to massive internal bleeding, hypovolemic shock and it is usually fatal.
Abdominal aortic aneurysms: as the thoracic aneurysms, they begin asymptomatic but may cause symptoms as they grow and compress surrounding structures.[18]Even though they usually remain asymptomatic, when they rupture they present with an ensuing mortality of 85 to 90%., and symptomatic patients require urgent surgical repair.[19]
When symptomatic, abdominal aortic aneurysms present with:
- Pain: in the chest, abdomen, lower back, or flanks. It may radiate to the groin, buttocks, or legs. The pain characteristics vary and may be deep, aching, gnawing, or throbbing It may also last for hours or days, not affected by movement. Occasionally, certain positions can be more comfortable and alleviate the symptoms;
- Pulsating abdominal mass;
- Ischemia: "cold foot" or a black or blue painful toe. This is usually the presentation when an aneurysm forms a blood cloth and it releases emboli to the lower extremities;
- Fever or weight loss if caused by inflammatory states such as vasculitis.[18]
If ruptured, the abdominal aortic aneurysm can present with sharp abdominal pain, often radiating to the back, discoloration of the skin and mucosa, tachycardia and low blood pressure due to hypovolemic shock.
Differential diagnosis include causes of pulsatile abdominal mass and/or abdominal pain such as ruptured viscus, strangulated hernia, ruptured visceral artery aneurysms, mesenteric ischemia, acute cholecystitis, ruptured hepatobiliary cancer, acute pancreatitis, lymphoma, and diverticular abscess.[13]
Physical Examination
- Patients with ruptured AAA usually appear sick and in shock.
- Physical examination may be remarkable for:
- Pulsatile abdominal mass
- Hypotension
- Tachycardia
- Shock
- Cool extremities
- Diastolic murmur indicating aortic regurgitation from extension of TAA dissection
Laboratory Findings
- There are no specific laboratory findings associated with AAA.
- An abdominal ultrasound can be diagnostic of AAA and is the imaging tool used to screen for AAA.
- Anemia can be seen in ruptured AAA.
Imaging Findings
- An abdominal ultrasound can be diagnostic of AAA and is the imaging tool used to screen for AAA
- CTA/MRA can accurately demonstrate AAA extent.
Other Diagnostic Studies
- Conventional angiogram can be used to diagnose aortic aneurysms.
Treatment
Medical Therapy
- Statins are recommended in cases associated with atherosclerosis.
- Blood pressure control
Surgery
- The mainstay of therapy for AAA is aneurysmal repair if diameter>5.5cm or size increased>0.5cm over 6 months.
- Surgical repair is indicated in cases of TAA dissection and progressive enlargement.
Prevention
- Smoking cessation is an important measure to prevent AAA progression and rupture.
Related Chapters
References
- ↑ 1.0 1.1 1.2 1.3 Kuivaniemi, Helena, et al. "Understanding the pathogenesis of abdominal aortic aneurysms." Expert review of cardiovascular therapy 13.9 (2015): 975-987.
- ↑ Frederick, John R., and Y. Joseph Woo. "Thoracoabdominal aortic aneurysm." Annals of cardiothoracic surgery 1.3 (2012): 277.
- ↑ Livesay, James J., Gregory N. Messner, and William K. Vaughn. "Milestones in treatment of aortic aneurysm: Denton A. Cooley, MD, and the Texas Heart Institute." Texas Heart Institute Journal 32.2 (2005): 130.
- ↑ 4.0 4.1 4.2 Kuivaniemi, Helena, Chris D. Platsoucas, and M. David Tilson III. "Aortic aneurysms: an immune disease with a strong genetic component." Circulation 117.2 (2008): 242-252.
- ↑ Bhandari, R., Kanthi, Y. - The Genetics of Aortic Aneurysms - The American College of Cardiology - available at:https://www.acc.org/latest-in-cardiology/articles/2018/05/02/12/52/the-genetics-of-aortic-aneurysms
- ↑ Ruddy JM, Jones JA, Ikonomidis JS. Pathophysiology of thoracic aortic aneurysm (TAA): is it not one uniform aorta? Role of embryologic origin. Progress in cardiovascular diseases. 2013;56(1):68–73.
- ↑ Steed MM, Tyagi SC. Mechanisms of cardiovascular remodeling in hyperhomocysteinemia. Antioxidants & redox signaling. 2011;15(7):1927–1943.
- ↑ Bruemmer D, Daugherty A, Lu H, Rateri DL. Relevance of angiotensin II-induced aortic pathologies in mice to human aortic aneurysms. Ann N Y Acad Sci. 2011;1245:7–10.
- ↑ Gadson PF, Jr, Dalton ML, Patterson E, et al. Differential response of mesoderm- and neural crest-derived smooth muscle to TGF-beta1: regulation of c-myb and alpha1 (I) procollagen genes. Experimental cell research. 1997;230(2):169–180.
- ↑ Wolinsky H, Glagov S. Comparison of abdominal and thoracic aortic medial structure in mammals. Deviation of man from the usual pattern. Circulation research. 1969;25(6):677–686.
- ↑ Ailawadi G, Eliason JL, Upchurch GR Jr. Current concepts in the pathogenesis of abdominal aortic aneurysm. J Vasc Surg 2003;38:584-8.
- ↑ Thoracic Aneurysm Differential Diagnoses - Medscape available at: https://emedicine.medscape.com/article/761627-differential
- ↑ 13.0 13.1 13.2 Abdominal Aortic Aneurysm - Mayo Clinichttps://www.mayoclinic.org/diseases-conditions/abdominal-aortic-aneurysm/symptoms-causes/syc-20350688
- ↑ Ernst, Calvin B. "Abdominal aortic aneurysm." New England Journal of Medicine 328.16 (1993): 1167-1172.
- ↑ Thoracic Aortic Aneurysm - Mayo Clinic available at: https://www.mayoclinic.org/diseases-conditions/thoracic-aortic-aneurysm/symptoms-causes/syc-20350188
- ↑ Clift, Paul F., and Elena Cervi. "A review of thoracic aortic aneurysm disease." Echo Research and Practice 7.1 (2020): R1-R10.
- ↑ Hiller, H. G., and N. R. F. Lagattolla. "Thoracic aortic aneurysm presenting with dysphagia: a fatal delay in diagnosis." Thoracic surgical science 4 (2007).
- ↑ 18.0 18.1 Abdominal Aortic Aneurysm (AAA) Symptoms - Stanford Healthcare https://stanfordhealthcare.org/medical-conditions/blood-heart-circulation/abdominal-aortic-aneurysm/symptoms.html
- ↑ Kent, K. Craig. "Abdominal aortic aneurysms." New England journal of medicine 371.22 (2014): 2101-2108.
Template:WikiDoc Sources CME Category::Cardiology
- Hannawa KK, Eliason JL, Upchurch GR. Gender differences in abdominal aortic aneurysms. Vascular. 2009;17 Suppl 1(Suppl 1):S30-9.
- Gwon JG, Kwon TW, Cho YP, Han YJ, Noh MS. Analysis of in hospital mortality and long-term survival excluding in hospital mortality after open surgical repair of ruptured abdominal aortic aneurysm. Ann Surg Treat Res. 2016;91(6):303-308.
- Wilson CT1, Fisher E, Welch HG: Racial disparities in abdominal aortic aneurysm repair among male Medicare beneficiaries. Arch Surg. 2008 May;143(5):506-10. doi: 10.1001/archsurg.143.
- Livesay JJ, Messner GN, Vaughn WK. Milestones in the treatment of aortic aneurysm: Denton A. Cooley, MD, and the Texas Heart Institute. Tex Heart Inst J. 2005;32(2):130-4.
- Lindsay ME, Dietz HC. The genetic basis of aortic aneurysm. Cold Spring Harb Perspect Med. 2014;4(9):a015909. Published . doi:10.1101/cshperspect.a015909
- Lindsay ME, Dietz HC. Lessons on the pathogenesis of aneurysm from heritable conditions. Nature. 2011;473(7347):308-16.
- John R. Frederick, Y. Joseph Woo: Thoracoabdominal aortic aneurysm. Ann Cardiothorac Surg 2012;1(3):277-285.