Alpha 1-antitrypsin deficiency epidemiology and demographics
|
Alpha 1-antitrypsin deficiency Microchapters |
|
Differentiating Alpha 1-antitrypsin deficiency from other Diseases |
|---|
|
Diagnosis |
|
Treatment |
|
Case Studies |
|
Alpha 1-antitrypsin deficiency epidemiology and demographics On the Web |
|
American Roentgen Ray Society Images of Alpha 1-antitrypsin deficiency epidemiology and demographics |
|
FDA on Alpha 1-antitrypsin deficiency epidemiology and demographics |
|
CDC on Alpha 1-antitrypsin deficiency epidemiology and demographics |
|
Alpha 1-antitrypsin deficiency epidemiology and demographics in the news |
|
Blogs on Alpha 1-antitrypsin deficiency epidemiology and demographics |
|
Directions to Hospitals Treating Alpha 1-antitrypsin deficiency |
|
Risk calculators and risk factors for Alpha 1-antitrypsin deficiency epidemiology and demographics |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: Cafer Zorkun, M.D., Ph.D. [2]
Overview
Alpha 1-antitrypsin deficiency (A1AD) is more common in people of Northern European, Iberian, and Saudi Arabian descent. Most researchers believe it is markedly underrecognized.
Epidemiology and Demographics
People of northern European, Iberian and Saudi Arabian ancestry are at the highest risk for A1AD. Four percent carry the PiZ allele; between 1 in 625 and 1 in 2000 are homozygous.
<figure-inline><figure-inline>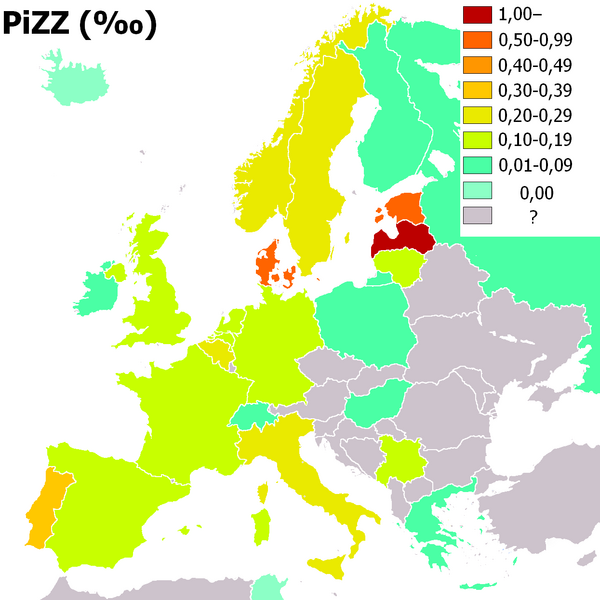 </figure-inline></figure-inline>
</figure-inline></figure-inline>
It is estimated that between 80,000 – 1000,000 (~ 1 in 1,650 to 1 in 3,000) Americans have severe alpha-1 AT deficiency (PI ZZ phenotype). This is approximately the same prevalence as cystic fibrosis. Studies have also estimated that ~ 2-3% of patients with severe COPD (chronic obstructive pulmonary disease) have severe alpha-1 AT deficiency. Given this relatively high prevalence, it is interesting to find that most clinicians perceive alpha-1 AT deficiency to be rare. In fact, only ~ 4% of patients with the PI ZZ phenotype were identified by the medical community in one study. The remaining 96% of PI ZZ patients must therefore be asymptomatic, or symptomatic but have escaped detection. In a recent survey, the average time interval between the onset of pulmonary symptoms and time of diagnosis was 7.2 years. Additionally, 43% of patients see at least 3 physicians before the diagnosis is established, and 12% see between 6 and 10. Thus, most authors believe that alpha-1 AT deficiency is markedly underrecognized. Because there are genetic implications to the next generation, that diagnosis can assist in smoking prevention / cessation, and that treatment is now available, enhanced detection is essential.
Frequency\
In United States, AATD is one of the most common lethal genetic diseases in adult white persons, with an incidence of 1/5000 individuals and prevalence of 70,000 to 100,000. About 25 million people carry atleast 1 deficient gene.
International
AATD is most common in Northern European and Iberian descends . Among white persons worldwide, there are an estimated 117 million carriers and 3.4 million affected individuals.
Race
White persons constitute an estimated 117 million carriers and 3.4 million affected individuals. Racial groups other than whites are affected less frequently.
Sex
Women and men are affected in equal numbers.
Age
The enzyme deficiency is congenital and has a bimodal distribution with respect to symptoms. It can be seen in neonates as a cause of neonatal jaundice and hepatitis. It can present in infants as cholestatic jaundice and in children as hepatic cirrhosis or liver failure. AATD is also the leading underlying condition requiring liver transplantation in children.
In adults, AATD leads to chronic liver disease in the fifth decade of life. As a cause of emphysema, it is seen in nonsmokers in the fifth decade of life and during the fourth decade of life in smokers.