African trypanosomiasis: Difference between revisions
Ethanleeman (talk | contribs) No edit summary |
Ethanleeman (talk | contribs) No edit summary |
||
| Line 16: | Line 16: | ||
{{SI}} | {{SI}} | ||
'''For patient information click [[ | '''For patient information click [[Sleeping sickness (patient information)|here]]''' | ||
{{Editor Help}} | {{Editor Help}} | ||
Revision as of 14:34, 24 June 2010
Template:DiseaseDisorder infobox
For patient information click here
Please Take Over This Page and Apply to be Editor-In-Chief for this topic: There can be one or more than one Editor-In-Chief. You may also apply to be an Associate Editor-In-Chief of one of the subtopics below. Please mail us [1] to indicate your interest in serving either as an Editor-In-Chief of the entire topic or as an Associate Editor-In-Chief for a subtopic. Please be sure to attach your CV and or biographical sketch.
Overview
Sleeping sickness or African trypanosomiasis is a parasitic disease in people and animals, caused by protozoa of genus Trypanosoma and transmitted by the tsetse fly. The disease is endemic in certain regions of Sub-Saharan Africa, covering about 36 countries and 60 million people. It is estimated that 50,000 to 70,000 people are currently infected, the number having declined somewhat in recent years.[1] The condition has been present in Africa since at least the 14th century, and probably for thousands of years before that. The causative agent and vector were not identified until 1902–1903 by Sir David Bruce, and the differentiation between protozoa was not made until 1910. The first effective treatment, Atoxyl, an arsenic based drug developed by Paul Ehrlich and Kiyoshi Shiga was introduced in 1910 but blindness was a serious side effect. Numerous drugs designed to treat the disease have been introduced since then.
There have been three severe epidemics in Africa over the last century: one between 1896 and 1906, mostly in Uganda and the Congo Basin, one in 1920 in several African countries, and one that began in 1970 and is still in progress. The 1920 epidemic was arrested due to mobile teams systematically screening millions of people at risk. The disease had practically disappeared between 1960 and 1965. After that success, screening and effective surveillance were relaxed and the disease has reappeared in endemic form in several foci over the last thirty years. [2]
There are two types of African trypanosomiasis; each is named for the region of Africa in which they are found:
- East african trypanosomiasis
- West african trypanosomiasis
Also known as:
Sleeping Sickness[3]
Epidemiology and Demographics
The disease is found in two forms, depending on the parasite, either Trypanosoma brucei gambiense or Trypanosoma brucei rhodesiense. T. b. gambiense is found in central and western Africa; it causes a chronic condition that can extend in a passive phase for months or years before symptoms emerge. T. b. rhodesiense, is the acute form of the disease but has a much more limited range. It is found in southern and eastern Africa; its infection emerges in a few weeks and is more virulent and faster developing. According to recent estimates, the disability adjusted life years (9 to 10 years) (DALYs) lost due to sleeping sickness are 2.0 million.[4] Recent estimates indicate that over 60 million people living in some 250 foci are at risk of contracting the disease, and there are about 300,000 new cases each year.[5] The disease has been recorded as occurring in 36 countries, all in sub-Saharan Africa.
Humans are the main reservoir for Trypanosoma brucei gambiense, but this species can also be found in pigs and other animals. Wild game animals and cattle are the main reservoir of T. b. rhodesiense.
Horse-flies (Tabanidae) and Stomoxydinae possibly could play a role by mechanical transmission (in special situations) not only of Nagana (the animal form of sleeping sickness) but also of the human disease form.[6]
East african trypanosomiasis
Worldwide, approximately 25,000 new cases of both East and West African trypanosomiasis are reported to the World Health Organization each year. However, many cases are not reported due to a lack of infrastructure and the true number of new cases is undoubtedly much higher. Since 1967, thirty-six cases of East African trypanosomiasis have been reported within the United States, all among individuals who had traveled to Africa.
East African trypanosomiasis is found in parts of Eastern and Central Africa, including Uganda, Kenya, Tanzania, Malawi, Ethiopia, Zaire, Zimbabwe, and Botswana. Areas where infection is spread are largely determined by the location of the infected tsetse fly and wild animal population.
West african trypanosomiasis
Worldwide, approximately 40,000 new cases of both East and West African trypanosomiasis are reported to the World Health Organization each year. However, the majority of cases are not reported due to a lack of infrastructure and it is likely that there are more than 100,000 new cases annually. Few cases of West African trypanosomiasis have been reported in the United States.
West African trypanosomiasis can be contracted in parts of Western and Central Africa. The tsetse fly lives only in Africa; areas where infection is spread are largely determined by where the infected tsetse fly is found.[7]
Risk Factors
East african trypanosomiasis
East African trypanosomiasis is usually found in woodland and savannah areas away from human habitation. Tourists, hunters, game wardens, and other persons working or visiting game parks in East and Central Africa are at greatest risk for illness.
West african trypanosomiasis
Tsetse flies can be found in Western and Central African forests, in areas of thick shrubbery and trees by rivers and waterholes. Risk of infection increases with the number of times a person is bitten by the tsetse fly. Therefore, tourists are not at great risk for contracting West African trypanosomiasis unless they are traveling and spending long periods of time in rural areas of Western and Central Africa.[8]
In addition to the bite of the tsetse fly, the disease is contractible in the following ways:
- Mother to child infection: the trypanosome can cross the placenta and infect the fetus, causing perinatal death.
- Laboratories: accidental infections, for example, through the handling of blood of an infected person and organ transplantation, although this is uncommon.
- Blood transfusion
Pathophysiology & Etiology
Protozoan hemoflagellates belonging to the complex Trypanosoma brucei. Two subspecies that are morphologically indistinguishable cause distinct disease patterns in humans: T. b. gambiense causes West African sleeping sickness and T. b. rhodesiense causes East African sleeping sickness. (A third member of the complex, T. b. brucei, under normal conditions does not infect humans.)
Infection occurs in 3 stages. A trypanosomal chancre can develop on the site of inoculation. This is followed by a hemolymphatic stage with symptoms that include fever, lymphadenopathy, and pruritus. In the meningoencephalitic stage, invasion of the central nervous system can cause headaches, somnolence, abnormal behavior, and lead to loss of consciousness and coma. The course of infection is much more acute with T. b. rhodesiense than T. b. gambiense.

The tsetse fly is large, brown and stealthy. The bite feels like a hot needle being stuck into the flesh. During a blood meal on the mammalian host, an infected tsetse fly (genus Glossina) injects metacyclic trypomastigotes into skin tissue. The parasites enter the lymphatic system and pass into the bloodstream 1. Inside the host, they transform into bloodstream trypomastigotes 2, are carried to other sites throughout the body, reach other blood fluids (e.g., lymph, spinal fluid), and continue the replication by binary fission 3. The entire life cycle of African Trypanosomes is represented by extracellular stages. The tsetse fly becomes infected with bloodstream trypomastigotes when taking a blood meal on an infected mammalian host (4,5). In the fly’s midgut, the parasites transform into procyclic trypomastigotes, multiply by binary fission 6, leave the midgut, and transform into epimastigotes 7. The epimastigotes reach the fly’s salivary glands and continue multiplication by binary fission 8. The cycle in the fly takes approximately 3 weeks. Humans are the main reservoir for Trypanosoma brucei gambiense, but this species can also be found in animals. Wild game animals are the main reservoir of T. b. rhodesiense.
East african trypanosomiasis
The disease is caused by a parasite named Trypanosoma brucei rhodesiense (tri-PAN-o-SO-ma BREW-see-eye rho-DEE-see-ense), carried by the tsetse fly. An individual will get East African trypanosomiasis if they are bitten by a tsetse fly infected with the Trypanosoma brucei rhodesiense parasite. The tsetse fly is common only to Africa.
West african trypanosomiasis
West African trypanosomiasis, also called Gambian sleeping sickness, is caused by a parasite called Trypanosoma brucei gambiense (tri-PAN-o-SO-ma BREW-see-eye GAM-be-ense) carried by the tsetse fly. An individual gets West African trypanosomiasis through the bite of an infected tsetse fly, found only in Africa. On rare occasions, a pregnant woman may pass the infection to her baby, or an individual may become infected through a blood transfusion or organ transplant.[9]
Diagnosis
- If you suspect that you may have East African trypanosomiasis, immediately consult with your health care provider who will order several tests to look for the parasite. Common tests include blood samples, a spinal tap, and skin biopsies, especially if you have a chancre.
- If you suspect that you may have West African trypanosomiasis, see your health care provider who will order several tests to look for the parasite. Common tests include blood samples and a spinal tap. Your physician may also take a sample of fluid from swollen lymph nodes.[10]
History and Symptoms
A bite by the tsetse fly is often painful and can develop into a red sore, also called a chancre (SHAN-ker).Symptoms begin within 1 to 4 weeks of getting an infected tsetse fly bite and begin with fever, headaches, and joint pains. As the parasites enter through both the blood and lymph systems, lymph nodes often swell up to tremendous sizes. Winterbottom's sign, the telltale swollen lymph glands along the back of the neck may appear. If untreated, the disease slowly overcomes the defenses of the infected person, and symptoms spread to include anemia, endocrine, cardiac, and kidney diseases and disorders. The disease then enters a neurological phase when the parasite passes through the blood-brain barrier. The symptoms of the second phase give the disease its name; besides confusion and reduced coordination, the sleep cycle is disturbed with bouts of fatigue punctuated with manic periods progressing to daytime slumber and nighttime insomnia. Without treatment, the disease is fatal, with progressive mental deterioration leading to coma and death. Damage caused in the neurological phase can be irreversible.
Laboratory Findings
The diagnosis rests upon demonstrating trypanosomes by microscopic examination of chancre fluid, lymph node aspirates, blood, bone marrow, or, in the late stages of infection, cerebrospinal fluid. A wet preparation should be examined for the motile trypanosomes, and in addition a smear should be fixed, stained with Giemsa (or Field), and examined. Concentration techniques can be used prior to microscopic examination. For blood samples, these include centrifugation followed by examination of the buffy coat; mini anion-exchange/centrifugation; and the Quantitative Buffy Coat (QBC) technique. For other samples such as spinal fluid, concentration techniques include centrifugation followed by examination of the sediment. Isolation of the parasite by inoculation of rats or mice is a sensitive method, but its use is limited to T. b. rhodesiense. Antibody detection has sensitivity and specificity that are too variable for clinical decisions. In addition, in infections with T. b. rhodesiense, seroconversion occurs after the onset of clinical symptoms and thus is of limited use.
Three similar serological tests are available for detection of the parasite; the micro-CATT, wb-CATT, and wb-LATEX. The first uses dried blood while the other two use whole blood samples. A 2002 study found the wb-CATT to be the most efficient for diagnosis, while the wb-LATEX is a better exam for situations where greater sensitivity is required. PMID 12481210
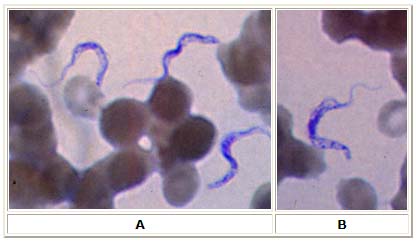
A, B: Two areas from a blood smear from a patient with African trypanosomiasis. Thin blood smear stained with Giemsa. Typical trypomastigote stages (the only stages found in patients), with a posterior kinetoplast, a centrally located nucleus, an undulating membrane, and an anterior flagellum. The two T. brucei species that cause human trypanosomiasis, T. b. gambiense and T. b. rhodesiense, are indistinguishable morphologically. The trypanosomes length range is 14 to 33 µm.
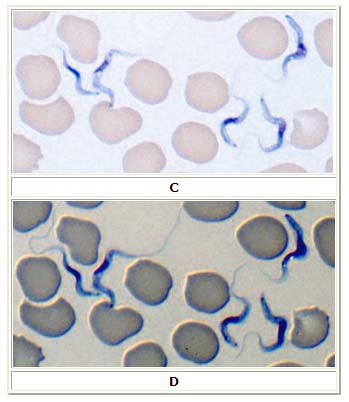
C, D: Blood smear from a patient with T. b. rhodesiense, Giemsa stain. D shows the same field as C, with the addition of differential interference contrast (DIC) which better visualizes the flagella (DIC is not necessary for diagnosis!). 41-year-old man who had returned from a trip to Tanzania. Specimen contributed by Dr. Phil Smith, Omaha, Nebraska.
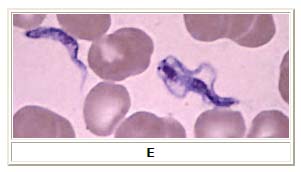
E: Blood smear from a patient (a U.S. traveler) with T. b. rhodesiense. A dividing parasite is seen at the right. Dividing forms are seen in African trypanosomiasis, but not in American trypanosomiasis (Chagas disease).
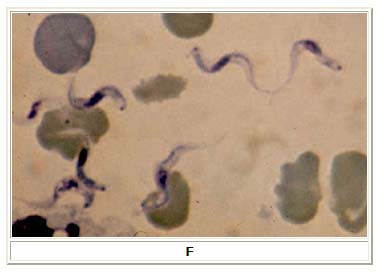
F: Blood smear from a patient with T. b. gambiense. Image contributed by Prof. J. Le Bras, Hôpital Bichat - Claude Bernard, Paris, France.
Risk Stratification and Prognosis
- No one is immune from East African trypanosomiasis. Even if you had the disease once, you can get re-infected.[11]
Treatment
- Medical treatment of East African trypanosomiasis should begin as soon as possible and is based on the infected person’s symptoms and laboratory results. Medication for the treatment of East African trypanosomiasis is available through the CDC. Hospitalization for treatment is necessary. Periodic follow-up exams that include a spinal tap are required for 2 years. If a person fails to receive medical treatment for East African trypanosomiasis, death will occur within several weeks to months.
- Medication for the treatment of West African trypanosomiasis is available. Hospitalized treatment of West African trypanosomiasis should begin as soon as possible and is based on the infected person’s symptoms and laboratory results. Hospitalization for treatment is necessary. Periodic follow-up exams that include a spinal tap are required for 2 years. West African trypanosomiasis is fatal if it is not treated.
Pharmacotherapy
Pentamidine isethionate and suramin (under an investigational New Drug Protocol from the CDC Drug Service) are the drugs of choice to treat the hemolymphatic stage of West and East African Trypanosomiasis, respectively. Melarsoprol is the drug of choice for late disease with central nervous system involvement (infections by T.b. gambiense or T. b. rhodiense). The current standard treatment for first stage disease is:
- Intravenous pentamidine (for T.b. gambiense); or
- Intravenous suramin (for T.b. rhodesiense)
The current standard treatment for second stage (late stage) disease is:
- Intravenous melarsoprol 2.2 mg/kg daily for 10 consecutive days.[13]
Alternative first line therapies include:
- Intravenous melarsoprol 0.6 mg/kg on day 1, 1.2 mg/kg iv melarsoprol on day 2, and 1.2 mg/kg/day iv melarsoprol combined with oral 7.5 mg/kg nifurtimox twice a day on days 3 to 10;[14] or
- Intravenous eflornithine 50 mg/kd every six hours for 14 days.[15]
In areas with melarsoprol resistance or in patients who have relapsed after melarsoprol monotherapy, the treatment should be:
- melarsoprol and nifurtimox, or
- eflornithine
The following traditional regimens should no longer be used:
- (old "standard" 26-day melarsoprol therapy) Intravenous melarsoprol therapy (3 series of 3.6 mg/kg/day intravenously for 3 days, with 7-day breaks between the series) (this regimen is less convenient and patients are less likely to complete therapy)[16];
- (incremental melarsoprol therapy) 10-day incremental-dose melarsoprol therapy (0.6 mg/kg iv on day 1, 1.2 mg/kg iv on day 2, and 1.8 mg/kg iv on days 3–10) (previously thought to reduce the risk of treatment-induced encephalopathy, but now known to be associated with an increased risk of relapse and a higher incidence of encephalopathy)[14][16];
According to a treatment study of Trypanosoma gambiense caused human African trypanosomiasis, use of eflornithine (DMFO) resulted in fewer adverse events than treatment with melaroprol. [17]
All patients should be followed up for two years with lumbar punctures every six months to look for relapse.
History of treatment for sleeping sickness
Suramin was introduced in 1920 to treat the first stage of the disease. By 1922, Suramin was generally combined with Tryparsamide (another pentavalent organo-arsenic drug) in the treatment of the second stage of the gambiense form. It was used during the grand epidemic in West and Central Africa in millions of people and was the mainstay of therapy until 1969.
Pentamidine, a highly effective drug for the first stage of the disease, has been used since 1939. During the fifties, it was widely used as a prophylactic agent in Western Africa, leading to a sharp decline in infection rates. At the time, it was thought that eradication of the disease was at hand.
The organo-arsenical melarsoprol (Arsobal) was developed in the 1940s, and is effective for patients with second stage sleeping sickness. However, 3 - 10% of those injected have reactive encephalopathy (convulsions, progressive coma, or psychotic reactions), and 10 - 70% die; it can cause brain damage in those that survive the encephalopathy. However, due to its effectiveness, melarsoprol is still used today. Resistance to melarsoprol is increasing, and combination therapy with nifurtimox is currently under research.
Eflornithine (difluoromethylornithine or DFMO), the most modern treatment, was developed in the 1970s by Albert Sjoerdsmanot and underwent clinical trials in the 1980s. The drug was approved by the United States Food and Drug Administration in 1990, but Aventis, the company responsible for its manufacture, halted production in 1999. In 2001, however, Aventis, in association with Médecins Sans Frontières and the World Health Organization, signed a long-term agreement to manufacture and donate the drug.
The genome of the parasite has been decoded and several proteins have been identified as potential targets for drug treatment. The decoded DNA also revealed the reason why generating a vaccine for this disease has been so difficult. T. brucei has over 800 genes that manufacture proteins that the disease mixes and matches to evade immune system detection.[18]
An international research team working in the Democratic Republic of the Congo, Southern Sudan and Angola involving Immtech International and University of North Carolina at Chapel Hill have completed a Phase IIb clinical trial and commenced a Phase III trial in 2005 testing the efficacy of the first oral treatment for Sleeping Sickness, known at this point as "DB289". [19] [20]
Recent findings indicate that the parasite is unable to survive in the bloodstream without its flagellum. This insight gives researchers a new angle with which to attack the parasite.[21]
A new treatment based on a truncated version of the apolipoprotein L-1 of high density lipoprotein and a nanobody has recently been found to work in mice, but has not been tested in humans.[22]
Prevention and control
Prevention and control focus on, where it is possible, the eradication of the parasitic host, the tsetse fly. Two alternative strategies have been used in the attempts to reduce the African trypanosomiases. One tactic is primarily medical or veterinary and targets the disease directly using monitoring, prophylaxis, treatment, and surveillance to reduce the number of organisms which carry the disease. The second strategy is generally entomological and intends to disrupt the cycle of transmission by reducing the number of flies. For in depth information on prevention of the disease via tsetse fly control see Tsetse fly control
Instances of sleeping sickness are being reduced by the use of the sterile insect technique.
Regular active surveillance, involving case detection and treatment, in addition to tsetse fly control, is the backbone of the strategy for control of sleeping sickness. Systematic screening of communities in identified foci is the best approach as case-by-case screening is not practically possible in highly endemic regions. Systematic screening may be in the form of mobile clinics or fixed screening centres where teams travel daily to the foci. The nature of gambiense disease is such that patients don't seek treatment early enough because the symptoms at that stage are not evident or serious enough to warrant seeking medical attention, considering the remoteness of some affected areas. Also, diagnosis of the disease is difficult and most health workers may not be able to detect it. Systematic screening allows early-stage disease to be detected and treated before the disease progresses, and removes the potential human reservoir.[23]
- There is neither a vaccine nor recommended drug available to prevent East African trypanosomiasis.
- There is neither a vaccine nor recommended drug available to prevent West African trypanosomiasis.
How can I prevent African trypanosomiasis and prevent other insect bites?
- Wear protective clothing, including long-sleeved shirts and pants. The tsetse fly can bite through thin fabrics, so clothing should be made of thick material.
- Wear khaki or olive colored clothing. The tsetse fly is attracted to bright colors and very dark colors.
- Use insect repellant. Though insect repellants have not proven effective in preventing tsetse fly bites, they are effective in preventing other insects from biting and causing illness.
- Use bed netting when sleeping.
- Inspect vehicles for tsetse flies before entering.
- Do not ride in the back of jeeps, pickup trucks or other open vehicles. The tsetse fly is attracted to the dust that moving vehicles and wild animals create.
- Avoid bushes. The tsetse fly is less active during the hottest period of the day. It rests in bushes but will bite if disturbed. [24]
Acknowledgements
The content on this page was first contributed by: C. Michael Gibson, M.S., M.D.
List of contributors:
Pilar Almonacid
References
- ↑ Template:Cite paper
- ↑ Template:Cite paper
- ↑ http://www.cdc.gov/ncidod/dpd/parasites/trypanosomiasis/factsht_ea_trypanosomiasis.htm
- ↑ Template:Cite paper
- ↑ Template:Cite paper
- ↑ Cherenet T, Sani RA, Panandam JM, Nadzr S, Speybroeck N, van den Bossche P (2004). "Seasonal prevalence of bovine trypanosomosis in a tsetse-infested zone and a tsetse-free zone of the Amhara Region, north-west Ethiopia". The Onderstepoort journal of veterinary research. 71 (4): 307&ndash, 312.
- ↑ http://www.cdc.gov/ncidod/dpd/parasites/trypanosomiasis/factsht_ea_trypanosomiasis.htm#what http://www.cdc.gov/ncidod/dpd/parasites/trypanosomiasis/factsht_wa_trypanosomiasis.htm
- ↑ http://www.cdc.gov/ncidod/dpd/parasites/trypanosomiasis/factsht_ea_trypanosomiasis.htm#what http://www.cdc.gov/ncidod/dpd/parasites/trypanosomiasis/factsht_wa_trypanosomiasis.htm#Top
- ↑ http://www.dpd.cdc.gov/dpdx/HTML/TrypanosomiasisAfrican.htm http://www.cdc.gov/ncidod/dpd/parasites/trypanosomiasis/factsht_ea_trypanosomiasis.htm#what http://www.cdc.gov/ncidod/dpd/parasites/trypanosomiasis/factsht_wa_trypanosomiasis.htm
- ↑ http://www.cdc.gov/ncidod/dpd/parasites/trypanosomiasis/factsht_ea_trypanosomiasis.htm#what http://www.cdc.gov/ncidod/dpd/parasites/trypanosomiasis/factsht_wa_trypanosomiasis.htm
- ↑ http://www.cdc.gov/ncidod/dpd/parasites/trypanosomiasis/factsht_ea_trypanosomiasis.htm#what
- ↑ http://www.cdc.gov/ncidod/dpd/parasites/trypanosomiasis/factsht_ea_trypanosomiasis.htm#what http://www.cdc.gov/ncidod/dpd/parasites/trypanosomiasis/factsht_wa_trypanosomiasis.htm#Top http://www.dpd.cdc.gov/dpdx/HTML/TrypanosomiasisAfrican.htm
- ↑ "Efficacy of new, concise schedule for melarsoprol in treatment of sleeping sickness caused by Trypanosoma brucei gambiense: a randomised trial". Lancet. 355 (9213): 1419&ndash, 25. 2000. PMID 10791526. Text " Burri C, Nkunku S, Merolle A, et al. " ignored (help)
- ↑ 14.0 14.1 Bisser S, N'Siesi F-X, Lejon V; et al. (2007). J Infect Dis. 195: 322&ndash, 29 http://www.journals.uchicago.edu/JID/journal/issues/v195n3/36827/36827.html. Missing or empty
|title=(help) - ↑ van Nieuwenhove S, Schechter PJ, Declercq J; et al. (1985). "Treatment of gambiense sleeping sickness in the Sudan with oral DFMO (DL-alfa-difluoromethyl ornithine) an inhibitor of ornithine decarboxylase: first field trial". Trans R Soc Trop Med Hyg. 79 (5): 692&ndash, 8.
- ↑ 16.0 16.1 Pepin J, Mpia B (2006). "Randomized controlled trial of three regimens of melarsoprol in the treatment of Trypanosoma brucei gambiense trypanosomiasis". Trans R Soc Trop Med Hyg. 100: 437&ndash, 41. PMID 16483622.
- ↑ Chappuis F, Udayraj N, Stietenroth K, Meussen A, Bovier PA (2005). "Eflornithine is safer than melarsoprol for the treatment of second-stage Trypanosoma brucei gambiense human African trypanosomiasis". Clin. Infect. Dis. 41 (5): 748–51. doi:10.1086/432576. PMID 16080099.
- ↑ Berriman M, Ghedin E, Hertz-Fowler C; et al. (2005). "The genome of the African trypanosome Trypanosoma brucei". Science. 309 (5733): 416–22. doi:10.1126/science.1112642. PMID 16020726.
- ↑ Williamson, David (August 25, 2005). "Compound might defeat African sleeping sickness, clinical trial beginning this month". University of North Carolina.
- ↑ Staff (September 15, 2005). "Clinical Trials Update". Genetic Engineering News. p. 5.
- ↑ "African Sleeping Sickness Breakthrough". Retrieved April 7. Unknown parameter
|accessyear=ignored (|access-date=suggested) (help); Check date values in:|accessdate=(help) - ↑ New Scientist, 25 Aug. 2007, pp. 35-7
- ↑ "Strategic Direction for African Trypanosomiasis Research". Special Programme for Research and Training in Tropical Diseases. Retrieved 2006-03-01.
- ↑ http://www.cdc.gov/ncidod/dpd/parasites/trypanosomiasis/factsht_ea_trypanosomiasis.htm#what http://www.cdc.gov/ncidod/dpd/parasites/trypanosomiasis/factsht_wa_trypanosomiasis.htm#Top
External links
- Sleeping sickness information page at Médecins Sans Frontières
- Drugs for Neglected Diseases Initiative
- Medecins Sans Frontieres' Eflornithine press release, 2001
- Links to pictures of Sleeping Sickness (Hardin MD/University of Iowa)
- The Sandler Center for Basic Research in Parasitic Diseases, University of California, San Francisco.
- Kids For World Health
ar:مرض النوم cs:Spavá nemoc da:Sovesyge de:Afrikanische Trypanosomiasis hr:Bolest spavanja it:Tripanosomiasi africana he:מחלת השינה nl:Slaapziekte no:Sovesyke simple:Sleeping sickness sk:Spavá choroba sr:Спаваћа болест fi:Unitauti
- CS1 maint: Multiple names: authors list
- Pages with citations using unnamed parameters
- Pages with citations lacking titles
- Pages with citations having bare URLs
- CS1 maint: Explicit use of et al.
- Pages with citations using unsupported parameters
- CS1 errors: dates
- Parasitic diseases
- DiseaseState
- Neurology
- Infectious disease