Adrenocortical carcinoma pathophysiology: Difference between revisions
No edit summary |
No edit summary |
||
| Line 12: | Line 12: | ||
The [[p53]] and retinoblastoma gene (RB) [[tumor suppressor gene]]s located on chromosomes 17p, 13q respectively, may be changed. The genes h19, insulin-like growth factor II (IGF-II), p57<sup>kip2</sup> are important for fetal growth and development. They are located on chromosome 11p. Expression of the h19 gene is markedly reduced in both nonfunctioning and functioning adrenal cortical carcinomas, especially in tumors producing [[cortisol]] and [[aldosterone]]. There is also a loss of activity of the p57<small>kip2</small> gene product in [[virilizing]] adenomas and adrenal cortical carcinomas. In contrast, IGF-II gene expression has been shown to be high in adrenal cortical carcinomas. Finally, c-myc gene expression is relatively high in neoplasms, and it is often linked to poor prognosis.<ref>{{cite book |author=Kufe D |editor=Benedict RC, Holland JF |title=Cancer medicine |publisher=B.C. Decker |location=Hamilton, Ont |year=2000 |edition=5th |isbn=1-55009-113-1 |oclc=156944448 }}</ref> | The [[p53]] and retinoblastoma gene (RB) [[tumor suppressor gene]]s located on chromosomes 17p, 13q respectively, may be changed. The genes h19, insulin-like growth factor II (IGF-II), p57<sup>kip2</sup> are important for fetal growth and development. They are located on chromosome 11p. Expression of the h19 gene is markedly reduced in both nonfunctioning and functioning adrenal cortical carcinomas, especially in tumors producing [[cortisol]] and [[aldosterone]]. There is also a loss of activity of the p57<small>kip2</small> gene product in [[virilizing]] adenomas and adrenal cortical carcinomas. In contrast, IGF-II gene expression has been shown to be high in adrenal cortical carcinomas. Finally, c-myc gene expression is relatively high in neoplasms, and it is often linked to poor prognosis.<ref>{{cite book |author=Kufe D |editor=Benedict RC, Holland JF |title=Cancer medicine |publisher=B.C. Decker |location=Hamilton, Ont |year=2000 |edition=5th |isbn=1-55009-113-1 |oclc=156944448 }}</ref> | ||
===Gross Pathology=== | ===Gross Pathology=== | ||
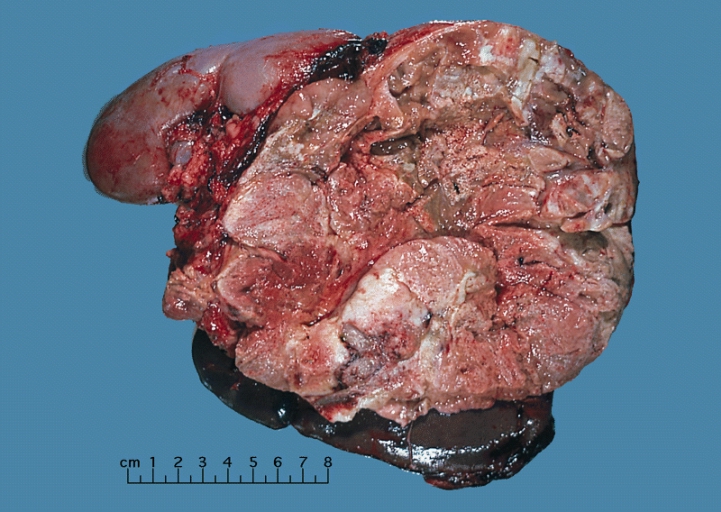
On gross pathology, adrenocortical carcinomas are often large, with a tan-yellow cut surface | On gross pathology, adrenocortical carcinomas are often large, with a tan-yellow cut surface and areas of [[hemorrhage]] and [[necrosis]]. | ||
[[Image:Adrenal_cortical_carcinoma.JPG|400px]] | [[Image:Adrenal_cortical_carcinoma.JPG|400px]] | ||
Revision as of 21:07, 27 August 2015
|
Adrenocortical carcinoma Microchapters |
|
Differentiating Adrenocortical carcinoma from other Diseases |
|---|
|
Diagnosis |
|
Treatment |
|
Case Study |
|
Adrenocortical carcinoma pathophysiology On the Web |
|
American Roentgen Ray Society Images of Adrenocortical carcinoma pathophysiology |
|
Risk calculators and risk factors for Adrenocortical carcinoma pathophysiology |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1] Associate Editor(s)-in-Chief: Raviteja Guddeti, M.B.B.S. [2]Shivali Marketkar, M.B.B.S. [3]Ahmad Al Maradni, M.D. [4]
Overview
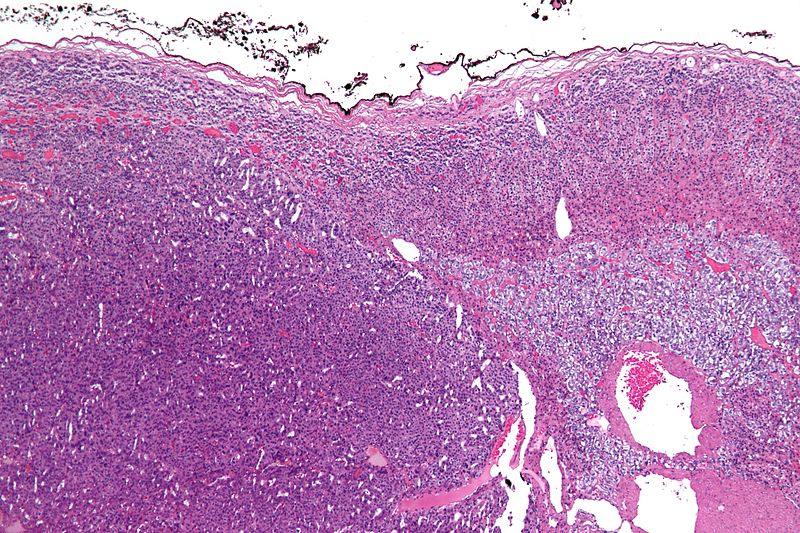
On gross pathology, a large tan-yellow surface with areas of hemorrhage and necrosis is a characteristic finding of adrenocortical carcinoma. On microscopic histopathological analysis, sheets of atypical cells with some resemblance to the cells of the normal adrenal cortex are a characteristic finding of adrenocortical carcinoma.
Pathophysiology
This tumor can produce the hormones cortisol, aldosterone, estrogen, or testosterone, as well as other hormones. In women the tumor often releases these hormones, which can lead to male characteristics. [Mutations]] of the tumor suppressor genes TP53 and TP57 might also be possible contributing factors for the development of adrenocortical carcinoma.
Genetics
The p53 and retinoblastoma gene (RB) tumor suppressor genes located on chromosomes 17p, 13q respectively, may be changed. The genes h19, insulin-like growth factor II (IGF-II), p57kip2 are important for fetal growth and development. They are located on chromosome 11p. Expression of the h19 gene is markedly reduced in both nonfunctioning and functioning adrenal cortical carcinomas, especially in tumors producing cortisol and aldosterone. There is also a loss of activity of the p57kip2 gene product in virilizing adenomas and adrenal cortical carcinomas. In contrast, IGF-II gene expression has been shown to be high in adrenal cortical carcinomas. Finally, c-myc gene expression is relatively high in neoplasms, and it is often linked to poor prognosis.[1]
Gross Pathology
On gross pathology, adrenocortical carcinomas are often large, with a tan-yellow cut surface and areas of hemorrhage and necrosis.
Shown above is a large adrenal cortical carcinoma resected from a 27-year-old woman. The tumor measured 17 cm in diameter and invaded kidney and spleen which necessitated en bloc removal of these organs with tumor. Patient had evidence of virilization.
Microscopic Pathology
On microscopic examination, the tumor usually displays sheets of atypical cells with some resemblance to the cells of the normal adrenal cortex. The presence of invasion and mitotic activity help differentiate small cancers from adrenocortical adenomas.[2]
Micrograph of an adrenocortical carcinoma (left of image - dark blue) and the adrenal cortex it arose from (right-top of image - pink/light blue). Benign adrenal medulla is present (right-middle of image - gray/blue). H&E stain.
Video
Shown below is a video explaining the histology of adrenocortical carcinoma
{{#ev:youtube|7jMFENhPaOM}}
References
- ↑ Kufe D (2000). Benedict RC, Holland JF, ed. Cancer medicine (5th ed.). Hamilton, Ont: B.C. Decker. ISBN 1-55009-113-1. OCLC 156944448.
- ↑ Richard Cote, Saul Suster, Lawrence Weiss, Noel Weidner (Editor). Modern Surgical Pathology (2 Volume Set). London: W B Saunders. ISBN 0-7216-7253-1.