Acute cholecystitis pathophysiology
|
Acute cholecystitis Microchapters |
|
Diagnosis |
|---|
|
Treatment |
|
Case Studies |
|
Acute cholecystitis pathophysiology On the Web |
|
American Roentgen Ray Society Images of Acute cholecystitis pathophysiology |
|
Risk calculators and risk factors for Acute cholecystitis pathophysiology |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: Furqan M M. M.B.B.S[2]
Overview
Acute calculous cholecystitis is usually caused by the mechanical obstruction of the gallbladder due to gallstones. Acute acalculous cholecystitis is caused predominantly by the gallbladder stasis. Gallstones are the most common cause of physical obstruction of the gallbladder usually at the neck or in the cystic duct. Cholesterol gallstones are the most common type of gallstones. The obstruction causes an increased pressure as the gallbladder mucosa continues to produce mucus. This raised pressure may cause the venous congestion which is followed by the arterial congestion. Eventually, the raised pressure and stasis leads to the gallbladder ischemia and necrosis. Mechanical obstruction of the gallbladder as a result of polyps, malignancy, an infestation of the gallbladder with parasites, foreign bodies, and trauma may also lead to the acute cholecystitis. Acute cholecystitis is more common in siblings and first degree relatives of affected persons. Lith gene is involved in the pathogenesis of cholecystitis. Mutations in the hepatic cholesterol transporter ABCG8 also predispose an individual to the develop gallstones. Acute cholecystitis is associated with diabetes, insulin resistance, cardiovascular diseases, non-alcoholic fatty liver disease (NAFLD) and gastrointestinal malignancies. Microscopic histopathology shows edematous and hemorrhagic gallbladder wall, mucosal necrosis with neutrophil infiltration. Bile infiltration of the gallbladder wall and bile and leucocyte margination of blood vessels are specific findings for acalculous cholecystitis.
Pathophysiology
Pathogenesis
Inflammation of the gallbladder is termed as cholecystitis. Acute calculous cholecystitis is usually caused by the mechanical obstruction due to gallstones. Acute acalculous cholecystitis is caused predominantly by the gallbladder stasis. The pathogenesis of acute cholecystitis involves the following:[1][2][3][4][5][6][7][8][9][10][11]
- Obstruction of the gallbladder:
- Gallstones are the most common cause of physical obstruction of the gallbladder usually at the neck or in the cystic duct. The obstruction causes an increased pressure as the gallbladder mucosa continues to produce mucus. This raised pressure may cause the venous congestion which is followed by the arterial congestion. Eventually, the raised pressure and stasis leads to the gallbladder ischemia and necrosis.
- There are two major types of gallstones:
- Cholesterol gallstones:
- Cholesterol gallstones are the most predominant form of the gallstones. They account for approximately 80% of the total gallstones.
- The formation of gallstones is dependant on the following factors:
- Cholesterol supersaturation in the bile
- Crystal nucleation
- Gallbladder dysmotility
- Gallbladder absorption
- Pigmented gallstones:
- There are two types of pigmented gallstones.
- Black stones
- Black stones consist of calcium bilirubinate and mucin glycoproteins.
- Black stones are predominantly associated with hemolytic conditions or cirrhosis (as a result of increased levels of unconjugated bilirubin).
- These stones are usually located in the gallbladder.
- Brown stones
- Brown stones are usually associated with bacterial infection.
- Brown stones are usually located elsewhere in the biliary tree as opposed to the gallbladder.
- Black stones
- There are two types of pigmented gallstones.
- Cholesterol gallstones:
- There are two major types of gallstones:
- Mechanical obstruction of the gallbladder as a result of polyps, malignancy, an infestation of the gallbladder with parasites, foreign bodies, and trauma may also lead to the acute cholecystitis.
- Gallstones are the most common cause of physical obstruction of the gallbladder usually at the neck or in the cystic duct. The obstruction causes an increased pressure as the gallbladder mucosa continues to produce mucus. This raised pressure may cause the venous congestion which is followed by the arterial congestion. Eventually, the raised pressure and stasis leads to the gallbladder ischemia and necrosis.
- Gallbladder stasis:
- Gallbladder stasis is usually due to the lack of gallbladder stimulation and contractility.
- This leads to concentration of the bile salts with a build-up of pressure within the organ. An increased intraluminal pressure results in ischemia and necrosis of the gallbladder.
- The gallbladder stasis also facilitates the proliferation of the bacteria such as Escherichia coli, Klebsiella, Bacteroides, Proteus, Pseudomonas, and Enterococcus faecalis. This can also cause an inflammatory reaction in the gallbladder.
Genetics
- Acute cholecystitis is more common in siblings and first degree relatives of affected persons.[12][13]
- Lith gene is involved in the pathogenesis of cholecystitis.[6]
- Mutations in the hepatic cholesterol transporter ABCG8 also predispose an individual to the develop gallstones.[9]
Associated Conditions
The following conditions are associated with acute cholecystitis:[14]
- Diabetes
- Insulin resistance
- Cardiovascular diseases
- Non-alcoholic fatty liver disease (NAFLD)
- Gastrointestinal malignancies:
Gross Pathology
- On gross pathology, acute cholecystitis has the following features:[15][16][17][18][2]
- Enlarged/distended gallbladder
- Serosal or mucosal exudates
- Thickened wall with hemorrhage and edema
- Ulcers, pus, bile, and gallstones
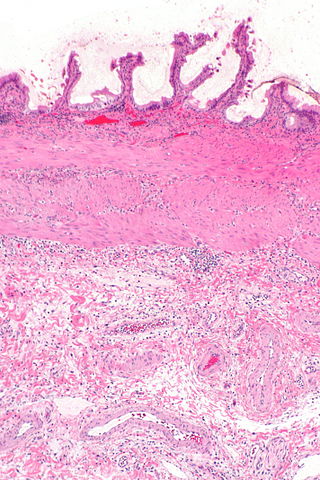
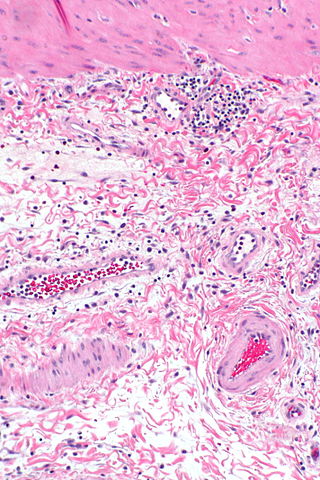
Microscopic Pathology
- On microscopic histopathological analysis, acute cholecystitis has the following features:[16][17][19][20]
- Edematous and hemorrhagic gallbladder wall
- Mucosal necrosis with neutrophil infiltration
- Eosinophilic infiltration of the gallbladder mucosa
- Specific microscopic features of acalculous cholecystitis:[15]
- Bile infiltration of gallbladder wall
- Bile infiltration and leucocyte margination of blood vessels
- Lymphatic dilation
 |
|
References
- ↑ Foard DE, Haber AH (1970). "Physiologically normal senescence in seedlings grown without cell division after massive gamma-irradiation of seeds". Radiat. Res. 42 (2): 372–80. PMID 5442405.
- ↑ 2.0 2.1 Jones MW, Ferguson T. "Gallbladder, Cholecystitis, Acalculous". PMID 29083717.
- ↑ Knab LM, Boller AM, Mahvi DM (2014). "Cholecystitis". Surg. Clin. North Am. 94 (2): 455–70. doi:10.1016/j.suc.2014.01.005. PMID 24679431.
- ↑ Yokoe M, Takada T, Strasberg SM, Solomkin JS, Mayumi T, Gomi H, Pitt HA, Gouma DJ, Garden OJ, Büchler MW, Kiriyama S, Kimura Y, Tsuyuguchi T, Itoi T, Yoshida M, Miura F, Yamashita Y, Okamoto K, Gabata T, Hata J, Higuchi R, Windsor JA, Bornman PC, Fan ST, Singh H, de Santibanes E, Kusachi S, Murata A, Chen XP, Jagannath P, Lee S, Padbury R, Chen MF (2012). "New diagnostic criteria and severity assessment of acute cholecystitis in revised Tokyo Guidelines". J Hepatobiliary Pancreat Sci. 19 (5): 578–85. doi:10.1007/s00534-012-0548-0. PMC 3429769. PMID 22872303.
- ↑ Yokoe M, Takada T, Strasberg SM, Solomkin JS, Mayumi T, Gomi H, Pitt HA, Garden OJ, Kiriyama S, Hata J, Gabata T, Yoshida M, Miura F, Okamoto K, Tsuyuguchi T, Itoi T, Yamashita Y, Dervenis C, Chan AC, Lau WY, Supe AN, Belli G, Hilvano SC, Liau KH, Kim MH, Kim SW, Ker CG (2013). "TG13 diagnostic criteria and severity grading of acute cholecystitis (with videos)". J Hepatobiliary Pancreat Sci. 20 (1): 35–46. doi:10.1007/s00534-012-0568-9. PMID 23340953.
- ↑ 6.0 6.1 Wang HH, Portincasa P, Afdhal NH, Wang DQ (2010). "Lith genes and genetic analysis of cholesterol gallstone formation". Gastroenterol. Clin. North Am. 39 (2): 185–207, vii–viii. doi:10.1016/j.gtc.2010.02.007. PMID 20478482.
- ↑ Loozen CS, Oor JE, van Ramshorst B, van Santvoort HC, Boerma D (2017). "Conservative treatment of acute cholecystitis: a systematic review and pooled analysis". Surg Endosc. 31 (2): 504–515. doi:10.1007/s00464-016-5011-x. PMID 27317033.
- ↑ Avegno J, Carlisle M (2016). "Evaluating the Patient with Right Upper Quadrant Abdominal Pain". Emerg. Med. Clin. North Am. 34 (2): 211–28. doi:10.1016/j.emc.2015.12.011. PMID 27133241.
- ↑ 9.0 9.1 Lammert F, Gurusamy K, Ko CW, Miquel JF, Méndez-Sánchez N, Portincasa P, van Erpecum KJ, van Laarhoven CJ, Wang DQ (2016). "Gallstones". Nat Rev Dis Primers. 2: 16024. doi:10.1038/nrdp.2016.24. PMID 27121416.
- ↑ Kimura Y, Takada T, Kawarada Y, Nimura Y, Hirata K, Sekimoto M, Yoshida M, Mayumi T, Wada K, Miura F, Yasuda H, Yamashita Y, Nagino M, Hirota M, Tanaka A, Tsuyuguchi T, Strasberg SM, Gadacz TR (2007). "Definitions, pathophysiology, and epidemiology of acute cholangitis and cholecystitis: Tokyo Guidelines". J Hepatobiliary Pancreat Surg. 14 (1): 15–26. doi:10.1007/s00534-006-1152-y. PMC 2784509. PMID 17252293.
- ↑ "Acute cholecystitis | The BMJ".
- ↑ "An Increased Familial Frequency of Gallstones - Gastroenterology".
- ↑ Weiss KM, Ferrell RE, Hanis CL, Styne PN (1984). "Genetics and epidemiology of gallbladder disease in New World native peoples". Am. J. Hum. Genet. 36 (6): 1259–78. PMC 1684666. PMID 6517051.
- ↑ Tiderington E, Lee SP, Ko CW (2016). "Gallstones: new insights into an old story". F1000Res. 5. doi:10.12688/f1000research.8874.1. PMC 4962289. PMID 27508070.
- ↑ 15.0 15.1 Laurila JJ, Ala-Kokko TI, Laurila PA, Saarnio J, Koivukangas V, Syrjälä H, Karttunen TJ (2005). "Histopathology of acute acalculous cholecystitis in critically ill patients". Histopathology. 47 (5): 485–92. doi:10.1111/j.1365-2559.2005.02238.x. PMID 16241996.
- ↑ 16.0 16.1 Owen CC, Bilhartz LE (2003). "Gallbladder polyps, cholesterolosis, adenomyomatosis, and acute acalculous cholecystitis". Semin. Gastrointest. Dis. 14 (4): 178–88. PMID 14719768.
- ↑ 17.0 17.1 McChesney JA, Northup PG, Bickston SJ (2003). "Acute acalculous cholecystitis associated with systemic sepsis and visceral arterial hypoperfusion: a case series and review of pathophysiology". Dig. Dis. Sci. 48 (10): 1960–7. PMID 14627341.
- ↑ Huang SM, Yao CC, Pan H, Hsiao KM, Yu JK, Lai TJ, Huang SD (2010). "Pathophysiological significance of gallbladder volume changes in gallstone diseases". World J. Gastroenterol. 16 (34): 4341–7. PMC 2937116. PMID 20818819.
- ↑ Kasprzak A, Malkowski W, Biczysko W, Seraszek A, Sterzyńska K, Zabel M (2011). "Histological alterations of gallbladder mucosa and selected clinical data in young patients with symptomatic gallstones". Pol J Pathol. 62 (1): 41–9. PMID 21574105.
- ↑ Yaylak F, Deger A, Bayhan Z, Kocak C, Zeren S, Kocak FE, Ekici MF, Algın MC (2016). "Histopathological gallbladder morphometric measurements in geriatric patients with symptomatic chronic cholecystitis". Ir J Med Sci. 185 (4): 871–876. doi:10.1007/s11845-015-1385-3. PMID 26602767.
- ↑ 21.0 21.1 "Acute cholecystitis - Libre Pathology".