Acute cardiac unloading

Acute Cardiac Unloading
Acute cardiac unloading is any maneuver, therapy, or intervention that decreases the power expenditure of the ventricle and limits the hemodynamic forces that lead to ventricular remodeling after insult or injury to the heart. The theory behind this approach to heart recovery is that by simultaneously limiting the oxygen demand and maximizing oxygen delivery to the heart after damage has occurred, the heart is more fully able to rest and recover. This is primarily achieved by using temporary minimally invasive mechanical circulatory support to supplant the pumping of blood by the heart. Using mechanical support decreases the workload of the heart, or unloads it. The scientific data supporting acute unloading as a method that promotes heart recovery is decades old. However, this approach was not technically feasible until the advent of miniaturized percutaneous left ventricular support devices, like the Impella (Abiomed, Inc.) in the early 2000s.
Cardiac traumas, such as myocardial infarction (commonly called a heart attack), myocarditis, peripartum cardiomyopathy, cardiogenic shock, and takotsubo cardiomyopathy, result in an impaired ability of the heart to pump blood. Without proper blood flow (also called cardiac output), all organ systems will eventually be starved of nutrients and oxygen, ultimately leading to organ death and death of the patient. Maintaining sufficient cardiac output is critical, and it is the primary objective of therapeutic approaches treating these cardiac traumas.
However, fundamental difficulties arise when applying currently indicated therapies aimed at increasing cardiac output. Often, these therapies increase both the stress placed on the heart and the risk to the patient. In the setting of decreased cardiac output due to damage to the heart, the heart itself is both the problem and the solution. Due to the damage, the heart is unable to pump a sufficient amount of blood. However, the only way to increase cardiac output is to further stress the already damaged heart. Thus begins a vicious cycle in which increased cardiac output is required, but in order to achieve this the damaged heart must work harder. This exacerbated stress leads to poorer outcomes in patients.[1][2][3][4][5][6][7][8][9] With the exception of cardiopulmonary bypass, current therapeutic approaches never allow the heart to rest and recover from injury. The workload of the heart (pumping blood) is never uncoupled from heart function. New approaches are needed. Acute cardiac unloading is able to functionally uncouple the heart from cardiac output thus allowing the heart to more fully rest and recover from damage.
Decreasing the Power Expenditure of the Heart by Acute Unloading
The heart actively pumps blood through the cardiovascular system. The pumping of blood is considered the workload of the heart and requires power expenditure. Acute cardiac unloading is any maneuver, therapy, or intervention that decreases the power expenditure of the ventricle while maintaining cardiac output. With few exceptions, oxygen is required for all biological processes that consume energy. Oxygen is used by biological systems to synthesize adenosine triphosphate (ATP) used in energy-consuming processes. Oxygen consumption (MVO2) is a direct measure of the total energy requirements of the heart, including the energy needed to pump blood.[10][11] An increase in MVO2 compared to resting conditions is indicative that the heart is working harder and is under stress.[10] Conversely, a decrease in MVO2 indicates that the heart is under a lesser amount of stress, and less energy is required to maintain proper blood flow. Therefore, decreased power expenditure directly correlates with a diminished MVO2.[10][11]
The Pressure-Volume Loop and MVO2 During Acute Unloading
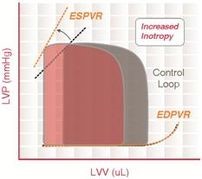

Pressure-volume (PV) loop analysis provides a framework for understanding MVO2 in the heart. The PV loop characterizes the events occurring during a single cardiac cycle (a single heartbeat). This tool is widely used in basic, pre-clinical, and clinical research to measure and visualize the mechanical work of the ventricle under various conditions.[12][13][14] With each cardiac cycle, the dynamic relationship between pressure and volume within the ventricle (typically the left ventricle) is plotted on an X-Y coordinate graph, resulting in a rounded trapezoidal shape commonly associated with PV loops. The loop is bounded on top by the end-systolic pressure-volume relationship (ESPVR) and on the bottom by the end-diastolic pressure-volume relationship (EDPVR). Both the ESPVR and EDPVR are intrinsic properties of the myocardium. The ESPVR defines the maximum pressure that the ventricle can develop at a given volume. As such, ESPVR is an index of ventricular contractility. The EDPVR describes the compliance of the myocardium. Both the ESPVR and EDPVR are dynamic properties and can change under physiological and pathophysiological conditions. The vertical lines that bound the left and right side of the loop represent isovolumic relaxation and contraction, respectively. The total area inside the loop is the mechanical energy (pressure-volume work) used to actively pump blood every beat, measured in mmHg·mL (aka, a joule). This is known as the stroke work (SW). The remaining area bound by the ESPVR and EDPVR that is outside of the loop is the potential energy (PE) that resides in the myofilaments that was not transduced into the work of pumping blood. The sum of these two areas (PE + SW) is known as the pressure-volume area (PVA). PVA is an excellent first-order approximation of MVO2.[10] Therefore, the PV loop provides valuable hemodynamic information as well as a measure of myocardial work.

As cardiac unloading is any maneuver, therapy, or intervention that decreases the workload and oxygen demand of the heart, unloading can be visualized as an overall decrease in the PVA of the PV loop. Mechanical unloading of the heart by a percutaneous transaortic device, such as the FDA-approved Impella pump (Abiomed, Inc., Danvers, MA), can achieve this in two ways.
First, the Impella is a continuous flow device. As such, it continuously aspirates blood directly from the ventricle into the aorta. This decreases the cardiac preload, and results in a left-shift and loss of the normal the isovolumic contraction line. The resulting PV loop is more triangular in shape, since at all stages of the cycle blood is being continuously pumped out of the ventricle. Second, as the level of circulatory support increases to higher flow rates and the ventricle becomes increasingly unloaded, the developed ventricular pressure drops. This is observed as a left-shift of end systolic pressure down the ESPVR line. As such, peak ventricular systolic and end-diastolic pressures are both reduced.[13]
Under normal physiological conditions, blood pressure in the aorta is primarily maintained by native cardiac output. Mean aortic pressure (MAP) is a key regulator of cardiovascular function and end-organ perfusion. Importantly, under conditions of mechanical support MAP is maintained independent of native ventricular function, and ventricular and aortic pressures become uncoupled.[15] Due to continuously unloading the ventricle of blood, the maximum developed LV pressure falls below MAP, and the aortic valve no longer opens. Cardiac output is maintained by the MCS device. When the aortic valve does not open, the heart no longer expends energy to actively pump blood and pressure-volume work is minimized. In this way, the entire PV loop is left-shifted, thus significantly decreasing the PVA.[16] Overall, MVO2 is spared, and cardiac output is maintained. The uncoupling of ventricular function from aortic pressure allows the heart to more completely rest and recover from damage.
While several studies dating from the early 1980s through the 1990s each suggested that unloading the heart during myocardial ischemia would be clinically beneficial, the practical application of this approach was not feasible given the medical technologies available at the time.[17][18][19][20][21][22] Research into the benefits of cardiac unloading was mostly relegated to basic and pre-clinical science; however, the development of new miniaturized percutaneous ventricular assist devices (pVADs) in the early 2000s enabled new and on-going investigations into the effect of unloading on infarct size.

Acute Cardiac Unloading and Myocardial Infarction
During a myocardial infarction, blood flow through one or more of the coronary arteries to a portion of the heart muscle is severely restricted or blocked altogether. This causes myocardial ischemia, or the restriction of blood supply leading to oxygen and nutrient deprivation. As with any tissue undergoing ischemia, when heart muscle becomes ischemic, it is damaged. If the duration of ischemia is long enough, this damage is irreversible and the tissue dies.
Unlike most other tissue types, the heart has an extremely limited innate ability to replace dead muscle with new, functional muscle.[23][24] When the heart is damaged by a myocardial infarction, a portion of muscle is permanently lost. The dead heart muscle is slowly replaced by non-contractile fibrotic tissue, forming what is called the myocardial scar. Scar tissue does not contract, and it does not help the heart pump blood. Therefore, the heart is functionally compromised. The remaining non-infarcted muscle must compensate for this loss and increase its function by structurally remodeling. This process is called ventricular remodeling. This persistently stresses the heart and increases the workload of the lasting myocardium. The amount of energy expended rises, measured by an increase in MVO2, and the heart is constantly stressed. While ventricular remodeling is initially an adaptive response that allows the heart to maintain proper cardiac output, it ultimately becomes maladaptive and can lead to heart failure.
Clinical research indicates that as the size of the myocardial scar increases, so does the likelihood of the patient to develop heart failure.[25][26] 1 in 4 patients will develop heart failure within 1 year of suffering a myocardial infarction, and 75% will develop heart failure within 5 years.[27] Therefore, limiting damage and scar formation resulting from ischemia is central to reducing the rate of heart failure development in heart attack patients.
To date, reperfusion therapy (the opening or bypassing of the blocked coronary artery) is the only intervention with demonstrated efficacy in limiting myocardial scar formation. In the clinic, reperfusion is typically accomplished through primary percutaneous coronary intervention (PCI) or coronary artery bypass grafting (CABG) surgery. Neither of these two interventions, however, can entirely prevent scar formation. While reperfusion is absolutely required to ensure the survival of some previously ischemic muscle tissue, it is estimated these therapies limit the final scar size by approximately 50% of the scar size that would form in the absence of any therapy.[28]
Decades of clinical research has focused on adjunctive therapeutics that may be used in parallel with reperfusion to further limit scar formation. These efforts have had very limited success, and no new therapies with demonstrated efficacy for limiting scar size have been adopted into the clinic in over 30 years.[29] Acute unloading is a new therapeutic approach aimed at limiting infarct scar size that is fundamentally different from previously attempted methods.
Targeting Myocardial Scar Formation with Acute Cardiac Unloading

Clinical and pre-clinical evidence indicates that the increased stress placed on the remaining viable myocardium after infarction leads to increased cell death. It is believed that cell death results, at least in part, from increased stresses placed on damaged--but still viable--myocardium. Physical (mechanical), oxidative, nutrient starvation, and other biomolecular stresses each play a role in inducing cardiomyocyte death post-infarct.[30][28][31] It is the loss of cardiomyocytes that weakens the function of the heart and leads to heart failure or death in the patient.
Acute cardiac unloading may help limit scar size through several independent but synergistic effects that address each of these stresses. First, acute unloading by MCS devices uncouples the workload of the heart from heart function and limits MVO2.[12][13][32] Second, the ability of these devices to maintain proper coronary perfusion pressure leads to increased nutrient and oxygen delivery and promotes cell survival during an ischemic event.[33][34] Third, mechanically unloading the ventricle decreases ventricular wall stress, a known pathological stimulus, that leads to ventricular remodeling and apoptosis.[31][35] Last, evidence suggests that these devices activate cardioprotective biochemical pathways within the heart.[31][32]
Limiting MVO2
pVADs, such as the Impella, can be temporarily implanted in the left ventricle to mechanically unload the heart. These transaortic axial pumps are capable of pumping blood at a rate as high as 5 L/min, which is equivalent to the average pumping rate of the resting human heart.[1] Therefore, by placing the pump into a patient suffering a myocardial infarction, the heart is unburdened of a significant portion of its workload. This results in a decrease in MVO2, and stress is alleviated from the heart.[12][13][16][32] Mechanical unloading is an energy sparing maneuver that results in the heart muscle having to work less to maintain cardiac output compared to the increased workload demanded of it during a myocardial infarction. By attenuating the physical stress placed on the heart, particularly the damaged but still viable muscle tissue at the edge of the expanding ischemic zone, the opportunity for the muscle to rest and recover is maximized.[36]
Increasing Perfusion Pressure
Beyond the effect of decreasing cardiac MVO2, another important effect of acute cardiac unloading is the maintenance of mean arterial blood pressure (MAP).[15] The pump actively aspirates blood from the ventricle directly into the aorta, thereby increasing aortic blood pressure. MAP is the driving force for end-organ blood perfusion, including the heart. After a myocardial infarction, the impaired ability of the heart to contract limits the capacity of the ventricle to develop pressure.[37] As a result, blood pressure drops. Consequently, coronary perfusion pressure decreases, further exacerbating myocardial ischemia and ischemia-dependent damage or cell death.[36] By maintaining MAP, acute cardiac unloading maintains coronary perfusion pressure.[33] This promotes oxygen and nutrient delivery to the remaining viable myocardium, thereby limiting further ischemia-dependent damage or cell death.

Decreasing Ventricular Wall Stress
This positive effect of mechanical support on perfusion pressure is further enhanced by the ability of the pump to decrease ventricular wall stress.[32] Post-infarct, the inability of the heart to efficiently pump blood leads to acute (and chronic) volume overload in the ventricular chambers. This places an additional outward force on the ventricle leading to compression of the coronary arteries. This compressive force increases vascular resistance, resulting in a further decrease in coronary blood flow and exacerbation of ischemia. Cell death follows. By physically unloading the ventricle of this excess blood volume, these compressive forces placed on the ventricular wall are relieved, and coronary vascular resistance is normalized.[32] Blood more freely flows into the myocardium—further aided by the increase in MAP brought about by mechanical support—and oxygen and nutrient supply is restored. Increased wall stress is also a known stimulus leading to cardiomyocyte apoptosis and maladaptive ventricular remodeling.[35] By relieving this stimulus, apoptosis and ventricular remodeling are blunted.
Cardioprotective Signaling
Evidence also indicates that acute cardiac unloading activates cardioprotective molecular signaling pathways. In 2015, Kapur and colleagues demonstrated unloading prior reperfusion activated discrete elements of both the Reperfusion Injury Salvage Kinase (RISK) and Survivor Activating Factor Enhancement (SAFE) pathways in a pig model of acute myocardial infarction.[32] This work also showed that acute unloading increased tissue and serum levels of stromal derived factor 1α and its cognate receptor, CXCR4, within the infarct zone; signals associated with cardioprotection and stem cell homing.[38] This data suggests that mechanical preconditioning of the heart prior to reperfusion is cardioprotective. A study by Li et al. in 2016 found that acute cardiac unloading also activates pro-survival FAK signaling and inhibits the activation of pro-apoptotic matrix metalloproteinase and c-Jun N-terminal kinase signaling.[31]
Acute Unloading Decreases Infarct Size in Pre-Clinical Studies
These synergistic effects of acute cardiac unloading are predicted to limit infarct scar size. Work from as early as 2003 demonstrated that left ventricular support by the Impella pump during ischemia and reperfusion significantly decreased infarct size and MVO2 while increasing myocardial blood supply in a sheep model of acute myocardial infarct.[39] In 2013, work by Wei and colleagues in a sheep model of chronic ischemia determined that unloading lead to a decreased infarct scar size associated with the normalization of ventricular wall strain, hemodynamic dysfunction, and cardiac Ca2+ handling.[40][41] That same year, the Kapur group established that mechanically unloading the heart prior to reperfusion using the Tandemheart device lead to a reduction in wall stress and infarct size in a pig model of acute myocardial infarct.[12] In 2015, the same group demonstrated a similar outcome using the simpler Impella device.[32] A similar outcome was independently observed by Sun et al. in 2015, also in a pig model of acute infarct and Impella support.[42] This group confirmed that mechanical unloading prior to reperfusion leads to smaller infarct sizes despite longer ischemic time.
The work by the Kapur and Sun groups helped establish the working hypothesis that acute unloading prior to reperfusion mechanically preconditions the heart and is an effective therapy for limiting infarct scar size in the setting of reperfusion. This hypothesis shifts the thinking away from primary reperfusion towards primary unloading. The focus of interventional cardiologists treating infarct patients is to reperfuse the blocked coronary artery as rapidly as possible. This focus is reflected in the commonplace adage, “Time is muscle.” The more time a tissue spends in ischemia, the more tissue will be permanently lost. In the 1990s and 2000s, significant effort was made to limit any delays in treating myocardial infarction. The American Heart Association and the American College of Cardiology guidelines recommend a “door-to-balloon” time of no more than 90 minutes. The current preclinical evidence indicates that even when the ischemic time is extended by up to 60 minutes (for a total ischemic time of 150 minutes), acute unloading prior to reperfusion still leads to a smaller infarct scar size compared to an ischemic time of 90 minutes. These data suggest that improvements in patient outcomes by applying acute unloading prior to reperfusion may be possible.
As of 2016, the clinical efficacy of primary unloading has not been directly tested. However, evidence for its effectiveness has been reported. In a retrospective registry study of 154 consecutive patients suffering from acute myocardial infarct complicated by cardiogenic shock who underwent PCI with Impella support, Dr. William O’Neill et al. reported that those patients who had Impella support initiated prior to PCI had significantly increased survival compared to those who had Impella support initiated after PCI.[43] It is important to note that infarct scar size was not measured in this study.
FDA Approval of the Door-To-Unloading Trial
In October of 2016, Abiomed, Inc. received FDA approval for the safety and feasibility “Door To Unloading” clinical trial.[2] This study will evaluate the use of the Impella CP heart pump for unloading of the left ventricle prior to primary PCI in patients presenting with STEMI without cardiogenic shock. The trial will focus on the feasibility and safety, and lay the groundwork for a future trial designed to measure the impact that acute unloading may have on infarct size related to reperfusion injury. This study is expected to begin patient enrollment in 2017.
A-CURE Working Group (Acute Cardiac Unloading and Recovery)

The Acute Cardiac Unloading and Recovery (A-CURE) Working Group is an association of leading experts in clinical and basic cardiac research convened in 2015 that is dedicated to advancing the science and clinical application of acute cardiac unloading. The intention of this multidisciplinary group is to develop the clinical, research, and educational tools necessary for the advancing acute cardiac unloading therapies. The central focus of the A-CURE Working Group is how best to leverage currently available and emerging medical technologies to develop new therapies aimed at heart muscle recovery after myocardial infarction or other cardiac traumas.
Current Faculty
- Mark Anderson, MD, Co-Chair (Hackensack University Medical Center)
- Daniel Burkhoff, MD, PhD, Co-Chair (Columbia University)
- Navin Kapur, MD, Co-Chair (Tufts Medical Center)
- Elazer Edelman, MD, PhD (Harvard University/Massachusetts Institute of Technology)
- Roger Hajjar, MD, PhD (Icahn School of Medicine at Mt. Sinai Hospital)
- Patrick Hunziker, MD (University of Basel)
- Kiyotake Ishikawa, MD (Icahn School of Medicine at Mt. Sinai Hospital
- Robert Kloner, MD, PhD (University of Southern California)
- Claudius Mahr, D.O. (University of Washington Medical Center)
- Bart Meyns, MD, PhD (KU Leuven)
- Jeff Moses, MD (Columbia University)
- Jacob Møller, MD, PhD (Odense University Hospital)
- William O'Neill, MD (Henry Ford Hospital)
- Eric Peterson, MD (Duke University)
- Andreas Schaefer, MD (Hannover Medical School)
- Kenji Sunagawa, MD, PhD (Kyushu University)
- Ryan Tedford, MD (Johns Hopkins Medicine)
- Nir Uriel, MD (University of Chicago)
- George Vetrovec, MD (Virginia Commonwealth University)
- Ralf Westenfeld (University of Dusseldorf)
Mission of the A-CURE Working Group
The mission of the A-CURE Working Group is to advance the science and mechanistic understanding of acute cardiac unloading and support the translation of basic and clinical research into therapies aimed at heart muscle recovery. The A-CURE Working Group was established in order to focus clinical, pre-clinical, and basic research efforts on how best to exploit emerging technologies and position them as therapies that maximize the ability of the heart to rest and recover after damage. The research of this group largely focuses on capitalizing on the hemodynamic and energetic benefits of acute cardiac unloading of the ventricle during and after a cardiac trauma. The group makes routine use of new percutaneous ventricular support devices such as the recently FDA approved Impella pump. A major research focus of the A-CURE Working Group is to develop new approaches to limit scar formation after a patient suffers a myocardial infarction.
History of The A-CURE Working Group
Investigations dating back to the 1960s have suggested that ventricular unloading before, during, or after the index ischemic event (heart attack) may positively affect cardiac function post-infarction.[17][20][44][45][46] However, unloading the ventricle through either mechanical or medical means was clinically impractical. Interest in unloading was limited. However, with the development of percutaneous left ventricular support devices (pLVAD) in the early 2000s interest in the therapeutic utility of acute ventricular unloading was invigorated.
In 2003, Meyns et al. published the first preclinical report demonstrating the effectiveness of unloading on myocardial infarct scar formation in the Journal of the American College of Cardiology.[39] Over the proceeding decade, several laboratories from around the world conducted independent investigations into the utility of and molecular mechanisms underlying acute cardiac unloading. The developing collaborations and communication amongst these laboratories formed the foundation of the A-CURE Working Group. Since 2015 the group has convened on a biannual basis in private meetings to discuss the current efforts of the individual labs and gain insight and feedback from the member groups. The 1st Annual A-CURE Public Symposium was held in Rome, Italy, on August 26th, 2016.[3] The A-CURE Public Symposium was attended by approximately 100 clinicians, scientists, and research professionals from 21 different countries. The meeting agenda featured keynote addresses by Dr. Eugene Braunwald (Founder of the TIMI Study Group, founding editor of Braunwald’s Heart Disease) and Dr. Joseph Hill (Editor-in-Chief of Circulation).[47] The 2nd Annual A-CURE Symposium was held on August 25, 2017, in Barcelona, Spain.[4] Dr. Valentin Fuster, MD, PhD Physician-in -Chief of the Mt. Sinai Hospital and Editor-in-Chief of the Journal of the American College of Cardiology gave the Keynote Address.
Past and future A-CURE Symposia
| Date | Location | Keynote Address |
|---|---|---|
| August 26, 2016 | Rome, Italy | Eugene Braunwald, MD
Joseph Hill, MD |
| August 25, 2017 | Barcelona, Spain | Valentin Fuster, MD, PhD |
| November 8, 2018 | Chicago, Illinois | TBD |
| TBD, 2019 | Paris, France | TBD |
| TBD, 2020 | Boston, Massachusetts | TBD |
Past and Future A-CURE Faculty Meetings
| Date | Location |
|---|---|
| January, 2015 | Paris, France |
| February, 2016 | Boston, Massachuesetts |
| January, 2017 | Boca Raton, Florida |
| March, 2018 | Orlando, Florida |
Current Efforts of The A-CURE Working Group
The A-CURE Working Group is currently focused on conducting the first clinical trial investigating the safety and feasibility of acute cardiac unloading for the treatment of myocardial infarction. The phase 1 clinical trial was recently approved by the FDA. A-CURE Faculty members Navin Kapur, MD (Tufts Medical Center, Boston) and William O’Neill, MD (Henry Ford Hospital, Detroit), and Jeffrey Moses, MD (Columbia University) are the steering committee for the study. The study is sponsored by Abiomed, Inc., the maker of the Impella pump.
External Links
www.A-CURE.org
www.Abiomed.com
www.texasheart.org/Research/Devices/tandemheart.cfm
Journal Of Cardiovascular Pharmacology and Therapeutics publication: http://cpt.sagepub.com/content/21/6
- ↑ 1.0 1.1 Rose, E. A. et al. Long-term use of a left ventricular assist device for end-stage heart failure. The New England journal of medicine 345, 1435-1443, doi:10.1056/NEJMoa012175 (2001).
- ↑ 2.0 2.1 Abraham, W. T. et al. In-hospital mortality in patients with acute decompensated heart failure requiring intravenous vasoactive medications: an analysis from the Acute Decompensated Heart Failure National Registry (ADHERE). Journal of the American College of Cardiology 46, 57-64, doi:10.1016/j.jacc.2005.03.051 (2005).
- ↑ 3.0 3.1 Bayram, M., De Luca, L., Massie, M. B. & Gheorghiade, M. Reassessment of dobutamine, dopamine, and milrinone in the management of acute heart failure syndromes. The American journal of cardiology 96, 47G-58G, doi:10.1016/j.amjcard.2005.07.021 (2005).
- ↑ 4.0 4.1 Cuffe, M. S. et al. Short-term intravenous milrinone for acute exacerbation of chronic heart failure: a randomized controlled trial. Jama 287, 1541-1547 (2002).
- ↑ Elkayam, U. et al. Use and impact of inotropes and vasodilator therapy in hospitalized patients with severe heart failure. American heart journal 153, 98-104, doi:10.1016/j.ahj.2006.09.005 (2007).
- ↑ Felker, G. M. et al. Heart failure etiology and response to milrinone in decompensated heart failure: results from the OPTIME-CHF study. Journal of the American College of Cardiology 41, 997-1003 (2003).
- ↑ Follath, F. et al. Efficacy and safety of intravenous levosimendan compared with dobutamine in severe low-output heart failure (the LIDO study): a randomised double-blind trial. Lancet 360, 196-202 (2002).
- ↑ Investigators, A. A. et al. Pexelizumab for acute ST-elevation myocardial infarction in patients undergoing primary percutaneous coronary intervention: a randomized controlled trial. Jama 297, 43-51, doi:10.1001/jama.297.1.43 (2007).
- ↑ Mebazaa, A. et al. Levosimendan vs dobutamine for patients with acute decompensated heart failure: the SURVIVE Randomized Trial. Jama 297, 1883-1891, doi:10.1001/jama.297.17.1883 (2007).
- ↑ 10.0 10.1 10.2 10.3 Burkhoff, D. & Naidu, S. S. The science behind percutaneous hemodynamic support: a review and comparison of support strategies. Catheterization and cardiovascular interventions : official journal of the Society for Cardiac Angiography & Interventions 80, 816-829, doi:10.1002/ccd.24421 (2012).
- ↑ 11.0 11.1 Suga, H. Total mechanical energy of a ventricle model and cardiac oxygen consumption. The American journal of physiology 236, H498-505 (1979).
- ↑ 12.0 12.1 12.2 12.3 Burkhoff, D. S., G.; Doshi, D., Uriel, N. Hemodynamics of Mechanical Circulatory Support. Journal of the American College of Cardiology 66, 2663-2674 (2015).
- ↑ 13.0 13.1 13.2 13.3 Kapur, N. K. et al. Mechanically unloading the left ventricle before coronary reperfusion reduces left ventricular wall stress and myocardial infarct size. Circulation 128, 328-336, doi:10.1161/CIRCULATIONAHA.112.000029 (2013).
- ↑ Klotz, S. et al. The impact of angiotensin-converting enzyme inhibitor therapy on the extracellular collagen matrix during left ventricular assist device support in patients with end-stage heart failure. Journal of the American College of Cardiology 49, 1166-1174, doi:10.1016/j.jacc.2006.10.071 (2007).
- ↑ 15.0 15.1 Verma, S., Burkhoff, D. & O'Neill, W. W. Avoiding hemodynamic collapse during high-risk percutaneous coronary intervention: Advanced hemodynamics of impella support. Catheterization and cardiovascular interventions : official journal of the Society for Cardiac Angiography & Interventions, doi:10.1002/ccd.26795 (2016).
- ↑ 16.0 16.1 Kapur, N. K. et al. Hemodynamic effects of left atrial or left ventricular cannulation for acute circulatory support in a bovine model of left heart injury. ASAIO journal 61, 301-306, doi:10.1097/MAT.0000000000000195 (2015).
- ↑ 17.0 17.1 Laschinger, J. C. et al. Adjunctive left ventricular unloading during myocardial reperfusion plays a major role in minimizing myocardial infarct size. The Journal of thoracic and cardiovascular surgery 90, 80-85 (1985).
- ↑ Muller, K. D., Sass, S., Gottwik, M. G. & Schaper, W. Effect of myocardial oxygen consumption on infarct size in experimental coronary artery occlusion. Basic research in cardiology 77, 170-181 (1982).
- ↑ Przyklenk, K. et al. Salvage of ischaemic myocardium by reperfusion: importance of collateral blood flow and myocardial oxygen demand during occlusion. Cardiovascular research 20, 403-414 (1986).
- ↑ 20.0 20.1 Van Winkle, D. M., Matsuki, T., Gad, N. M., Jordan, M. C. & Downey, J. M. Left ventricular unloading during reperfusion does not limit myocardial infarct size. Circulation 81, 1374-1379 (1990).
- ↑ Allen, B. S., Okamoto, F., Buckberg, G. D., Bugyi, H. & Leaf, J. Reperfusion conditions: critical importance of total ventricular decompression during regional reperfusion. The Journal of thoracic and cardiovascular surgery 92, 605-612 (1986).
- ↑ Axelrod, H. I. et al. Percutaneous cardiopulmonary bypass limits myocardial injury from ischemic fibrillation and reperfusion. Circulation 78, III148-152 (1988).
- ↑ Murry, C. E. & Lee, R. T. Development biology. Turnover after the fallout. Science 324, 47-48, doi:10.1126/science.1172255 (2009).
- ↑ Angert, D. et al. Repair of the injured adult heart involves new myocytes potentially derived from resident cardiac stem cells. Circulation research 108, 1226-1237, doi:10.1161/CIRCRESAHA.110.239046 (2011).
- ↑ Heusch, G. et al. Cardiovascular remodelling in coronary artery disease and heart failure. Lancet 383, 1933-1943, doi:10.1016/S0140-6736(14)60107-0 (2014).
- ↑ Stone, G. W. et al. Relationship Between Infarct Size and Outcomes Following Primary PCI: Patient-Level Analysis From 10 Randomized Trials. Journal of the American College of Cardiology 67, 1674-1683, doi:10.1016/j.jacc.2016.01.069 (2016).
- ↑ Ezekowitz, J. A. et al. Declining in-hospital mortality and increasing heart failure incidence in elderly patients with first myocardial infarction. Journal of the American College of Cardiology 53, 13-20, doi:10.1016/j.jacc.2008.08.067 (2009).
- ↑ 28.0 28.1 Hausenloy, D. J. & Yellon, D. M. Myocardial ischemia-reperfusion injury: a neglected therapeutic target. The Journal of clinical investigation 123, 92-100, doi:10.1172/JCI62874 (2013).
- ↑ Bulluck, H., Yellon, D. M. & Hausenloy, D. J. Reducing myocardial infarct size: challenges and future opportunities. Heart, doi:10.1136/heartjnl-2015-307855 (2015).
- ↑ Chiong, M. et al. Cardiomyocyte death: mechanisms and translational implications. Cell Death Dis 2, e244, doi:10.1038/cddis.2011.130 (2011).
- ↑ 31.0 31.1 31.2 31.3 Li, T. et al. Left Ventricular Unloading After Acute Myocardial Infarction Reduces MMP/JNK Associated Apoptosis and Promotes FAK Cell-Survival Signaling. The Annals of thoracic surgery, doi:10.1016/j.athoracsur.2016.05.007 (2016).
- ↑ 32.0 32.1 32.2 32.3 32.4 32.5 32.6 Kapur, N. K. et al. Mechanical Pre-Conditioning With Acute Circulatory Support Before Reperfusion Limits Infarct Size in Acute Myocardial Infarction. JACC. Heart failure 3, 873-882, doi:10.1016/j.jchf.2015.06.010 (2015).
- ↑ 33.0 33.1 Remmelink, M. et al. Effects of left ventricular unloading by Impella recover LP2.5 on coronary hemodynamics. Catheterization and cardiovascular interventions : official journal of the Society for Cardiac Angiography & Interventions 70, 532-537, doi:10.1002/ccd.21160 (2007).
- ↑ Sauren, L. D. et al. Combined Impella and intra-aortic balloon pump support to improve both ventricular unloading and coronary blood flow for myocardial recovery: an experimental study. Artificial organs 31, 839-842, doi:10.1111/j.1525-1594.2007.00477.x (2007).
- ↑ 35.0 35.1 Di Napoli, P. et al. Left ventricular wall stress as a direct correlate of cardiomyocyte apoptosis in patients with severe dilated cardiomyopathy. American heart journal 146, 1105-1111, doi:10.1016/S0002-8703(03)00445-9 (2003).
- ↑ 36.0 36.1 Reimer, K. A. & Jennings, R. B. The "wavefront phenomenon" of myocardial ischemic cell death. II. Transmural progression of necrosis within the framework of ischemic bed size (myocardium at risk) and collateral flow. Laboratory investigation; a journal of technical methods and pathology 40, 633-644 (1979).
- ↑ Pfeffer, M. A. et al. Myocardial infarct size and ventricular function in rats. Circulation research 44, 503-512 (1979).
- ↑ Davidson, S. M. et al. Remote ischaemic preconditioning involves signalling through the SDF-1alpha/CXCR4 signalling axis. Basic research in cardiology 108, 377, doi:10.1007/s00395-013-0377-6 (2013).
- ↑ 39.0 39.1 Meyns, B., Stolinski, J., Leunens, V., Verbeken, E. & Flameng, W. Left ventricular support by catheter-mounted axial flow pump reduces infarct size. Journal of the American College of Cardiology 41, 1087-1095 (2003).
- ↑ Bers, D. M. Excitation-Contraction Coupling and Cardiac Contractile Force. (Kluwer Academic Publishers, 2001).
- ↑ Wei, X. et al. Short-term mechanical unloading with left ventricular assist devices after acute myocardial infarction conserves calcium cycling and improves heart function. JACC. Cardiovascular interventions 6, 406-415, doi:10.1016/j.jcin.2012.12.122 (2013).
- ↑ Sun, X. et al. Early Assistance With Left Ventricular Assist Device Limits Left Ventricular Remodeling After Acute Myocardial Infarction in a Swine Model. Artificial organs 40, 243-251, doi:10.1111/aor.12541 (2016).
- ↑ O'Neill, W. W. et al. The current use of Impella 2.5 in acute myocardial infarction complicated by cardiogenic shock: results from the USpella Registry. Journal of interventional cardiology 27, 1-11, doi:10.1111/joic.12080 (2014).
- ↑ Levine, H. J., McIntyre, K. M. & Glovsky, M. M. Relief of angina pectoris by Valsalva maneuver. The New England journal of medicine 275, 487-489, doi:10.1056/NEJM196609012750907 (1966).
- ↑ Smalling, R. W. et al. Improved regional myocardial blood flow, left ventricular unloading, and infarct salvage using an axial-flow, transvalvular left ventricular assist device. A comparison with intra-aortic balloon counterpulsation and reperfusion alone in a canine infarction model. Circulation 85, 1152-1159 (1992).
- ↑ Laks, H. et al. The effect of left atrial-to-aortic assistance on infarct size. Circulation 56, II38-43 (1977).
- ↑ Braunwald, E., Mann, D.L., Bonow, R.O., Zipes, D.P., Libby, P. . Braunwald's Heart Disease: A Textbook of Cardiovascular Medicine - 10th Edition. (Elsevier Sauders, 2015).