Acarbose
{{DrugProjectFormSinglePage |authorTag=Gloria Picoy [1] |genericName=Acarbose |aOrAn=an |drugClass=alpha-glucosidase inhibitor |indicationType=treatment |indication=type 2 diabetes mellitus |adverseReactions=abdominal pain, Ddarrhea, flatulence |blackBoxWarningTitle=TITLE |blackBoxWarningBody=Condition Name: (Content) |fdaLIADAdult=Acarbose is indicated as an adjunct to diet and exercise to improve glycemic control in adults with type 2 diabetes mellitus.
- Dosage:
- Initial dosage: 25 mg given orally three times daily at the start (with the first bite) of each main meal.
- Maintenance dosage: Once a 25 mg t.i.d. dosage regimen is reached, dosage of acarbose should be adjusted at 4–8 week intervals based on one-hour postprandial glucose or glycosylated hemoglobin levels, and on tolerance.
|offLabelAdultGuideSupport=There is limited information regarding Off-Label Guideline-Supported Use of Acarbose in adult patients. |offLabelAdultNoGuideSupport=* Prophylaxis of type 2 diabetes mellitus |fdaLIADPed=Safety and efficacy not established in pediatric patients |offLabelPedGuideSupport=There is limited information regarding Off-Label Guideline-Supported Use of Acarbose in pediatric patients. |offLabelPedNoGuideSupport=There is limited information regarding Off-Label Non–Guideline-Supported Use of Acarbose in pediatric patients. |contraindications=Acarbose is contraindicated in patients with known hypersensitivity to the drug. Acarbose is contraindicated in patients with diabetic ketoacidosis or cirrhosis. Acarbose is also contraindicated in patients with inflammatory bowel disease, colonic ulceration, partial intestinal obstruction or in patients predisposed to intestinal obstruction. In addition, acarbose is contraindicated in patients who have chronic intestinal diseases associated with marked disorders of digestion or absorption and in patients who have conditions that may deteriorate as a result of increased gas formation in the intestine. |warnings=====Macrovascular Outcomes==== There have been no clinical studies establishing conclusive evidence of macrovascular risk reduction with acarbose or any other anti-diabetic drug.
Hypoglycemia
Because of its mechanism of action, acarbose when administered alone should not cause hypoglycemia in the fasted or postprandial state. Sulfonylurea agents or insulin may cause hypoglycemia. Because acarbose given in combination with a sulfonylurea or insulin will cause a further lowering of blood glucose, it may increase the potential for hypoglycemia. Hypoglycemia does not occur in patients receiving metformin alone under usual circumstances of use, and no increased incidence of hypoglycemia was observed in patients when acarbose was added to metformin therapy. Oral glucose (dextrose), whose absorption is not inhibited by acarbose, should be used instead of sucrose (cane sugar) in the treatment of mild to moderate hypoglycemia. Sucrose, whose hydrolysis to glucose and fructose is inhibited by acarbose, is unsuitable for the rapid correction of hypoglycemia. Severe hypoglycemia may require the use of either intravenous glucose infusion or glucagon injection.
Elevated Serum Transaminase Levels
In long-term studies (up to 12 months, and including acarbose doses up to 300 mg t.i.d.) conducted in the United States, treatment-emergent elevations of serum transaminases (AST and/or ALT) above the upper limit of normal (ULN), greater than 1.8 times the ULN, and greater than 3 times the ULN occurred in 14%, 6%, and 3%, respectively, of acarbose-treated patients as compared to 7%, 2%, and 1%, respectively, of placebo-treated patients. Although these differences between treatments were statistically significant, these elevations were asymptomatic, reversible, more common in females, and, in general, were not associated with other evidence of liver dysfunction. In addition, these serum transaminase elevations appeared to be dose related. In US studies including acarbose doses up to the maximum approved dose of 100 mg t.i.d., treatment-emergent elevations of AST and/or ALT at any level of severity were similar between acarbose-treated patients and placebo-treated patients (p ≥ 0.496).
In approximately 3 million patient-years of international postmarketing experience with acarbose, 62 cases of serum transaminase elevations > 500 IU/L (29 of which were associated with jaundice) have been reported. Forty-one of these 62 patients received treatment with 100 mg t.i.d. or greater and 33 of 45 patients for whom weight was reported weighed < 60 kg. In the 59 cases where follow-up was recorded, hepatic abnormalities improved or resolved upon discontinuation of acarbose in 55 and were unchanged in two. Cases of fulminant hepatitis with fatal outcome have been reported; the relationship to acarbose is unclear.
Loss of Control of Blood Glucose
When diabetic patients are exposed to stress such as fever, trauma, infection, or surgery, a temporary loss of control of blood glucose may occur. At such times, temporary insulin therapy may be necessary. |clinicalTrials=====Digestive Tract==== Gastrointestinal symptoms are the most common reactions to acarbose. In U.S. placebo-controlled trials, the incidences of abdominal pain, diarrhea, and flatulence were 19%, 31%, and 74% respectively in 1255 patients treated with acarbose 50–300 mg t.i.d., whereas the corresponding incidences were 9%, 12%, and 29% in 999 placebo-treated patients.
In a one-year safety study, during which patients kept diaries of gastrointestinal symptoms, abdominal pain and diarrhea tended to return to pretreatment levels over time, and the frequency and intensity of flatulence tended to abate with time. The increased gastrointestinal tract symptoms in patients treated with acarbose are a manifestation of the mechanism of action of acarbose and are related to the presence of undigested carbohydrate in the lower GI tract.
If the prescribed diet is not observed, the intestinal side effects may be intensified. If strongly distressing symptoms develop in spite of adherence to the diabetic diet prescribed, the doctor must be consulted and the dose temporarily or permanently reduced.
Elevated Serum Transaminase Levels
Other Abnormal Laboratory Findings: Small reductions in hematocrit occurred more often in acarbose-treated patients than in placebo-treated patients but were not associated with reductions in hemoglobin. Low serum calcium and low plasma vitamin B6 levels were associated with acarbose therapy but are thought to be either spurious or of no clinical significance. |postmarketing=Additional adverse events reported from worldwide postmarketing experience include fulminant hepatitis with fatal outcome, hypersensitive skin reactions (for example rash, erythema, exanthema and uticaria), edema, ileus/subileus, jaundice and/or hepatitis and associated liver damage, thrombocytopenia, and pneumatosis cystoides intestinalis.
Pneumatosis Cystoides Intestinalis
There have been rare postmarketing reports of pneumatosis cystoides intestinalis associated with the use of alpha-glucosidase inhibitors, including acarbose. Pneumatosis cystoides intestinalis may present with symptoms of diarrhea, mucus discharge, rectal bleeding, and constipation. Complications may include pneumoperitoneum, volvulus, intestinal obstruction, intussusception, intestinal hemorrhage, and intestinal perforation. If pneumatosis cystoides intestinalis is suspected, discontinue acarbose and perform the appropriate diagnostic imaging. |drugInteractions=Certain drugs tend to produce hyperglycemia and may lead to loss of blood glucose control. These drugs include the thiazides and other diuretics, corticosteroids, phenothiazines, thyroid products, estrogens, oral contraceptives, phenytoin, nicotinic acid, sympathomimetics, calcium channel-blocking drugs, and isoniazid. When such drugs are administered to a patient receiving acarbose, the patient should be closely observed for loss of blood glucose control. When such drugs are withdrawn from patients receiving acarbose in combination with sulfonylureas or insulin, patients should be observed closely for any evidence of hypoglycemia.
Patients Receiving Sulfonylureas or Insulin: Sulfonylurea agents or insulin may cause hypoglycemia. Acarbose given in combination with a sulfonylurea or insulin may cause a further lowering of blood glucose and may increase the potential for hypoglycemia. If hypoglycemia occurs, appropriate adjustments in the dosage of these agents should be made. Very rarely, individual cases of hypoglycemic shock have been reported in patients receiving acarbose therapy in combination with sulfonylureas and/or insulin.
Intestinal adsorbents (for example, charcoal) and digestive enzyme preparations containing carbohydrate-splitting enzymes (for example, amylase, pancreatin) may reduce the effect of acarbose and should not be taken concomitantly.
Acarbosehas been shown to change the bioavailability of digoxin when they are coadministered, which may require digoxin dose adjustment. |FDAPregCat=B |useInPregnancyFDA=The safety of acarbose in pregnant women has not been established. Reproduction studies have been performed in rats at doses up to 480 mg/kg (corresponding to 9 times the exposure in humans, based on drug blood levels) and have revealed no evidence of impaired fertility or harm to the fetus due to acarbose. In rabbits, reduced maternal body weight gain, probably the result of the pharmacodynamic activity of high doses of acarbose in the intestines, may have been responsible for a slight increase in the number of embryonic losses. However, rabbits given 160 mg/kg acarbose (corresponding to 10 times the dose in man, based on body surface area) showed no evidence of embryotoxicity and there was no evidence of teratogenicity at a dose 32 times the dose in man (based on body surface area). There are, however, no adequate and well-controlled studies of acarbose in pregnant women. Because animal reproduction studies are not always predictive of the human response, this drug should be used during pregnancy only if clearly needed. Because current information strongly suggests that abnormal blood glucose levels during pregnancy are associated with a higher incidence of congenital anomalies as well as increased neonatal morbidity and mortality, most experts recommend that insulin be used during pregnancy to maintain blood glucose levels as close to normal as possible. |useInNursing=A small amount of radioactivity has been found in the milk of lactating rats after administration of radiolabeled acarbose. It is not known whether this drug is excreted in human milk. Because many drugs are excreted in human milk, acarbose should not be administered to a nursing woman. |useInGeri=Of the total number of subjects in clinical studies of acarbose in the United States, 27% were 65 and over, while 4% were 75 and over. No overall differences in safety and effectiveness were observed between these subjects and younger subjects. The mean steady-state area under the curve (AUC) and maximum concentrations of acarbose were approximately 1.5 times higher in elderly compared to young volunteers; however, these differences were not statistically significant. |useInRenalImpair=Plasma concentrations of acarbose in renally impaired volunteers were proportionally increased relative to the degree of renal dysfunction. Long-term clinical trials in diabetic patients with significant renal dysfunction (serum creatinine > 2.0 mg/dL) have not been conducted. Therefore, treatment of these patients with acarbose is not recommended. |useInReproPotential=Fertility studies conducted in rats after oral administration produced no untoward effect on fertility or on the overall capability to reproduce. |administration=Oral |monitoring=Therapeutic response to acarbose should be monitored by periodic blood glucose tests. Measurement of glycosylated hemoglobin levels is recommended for the monitoring of long-term glycemic control.
Acarbose, particularly at doses in excess of 50 mg t.i.d., may give rise to elevations of serum transaminases and, in rare instances, hyperbilirubinemia. It is recommended that serum transaminase levels be checked every 3 months during the first year of treatment with acarbose and periodically thereafter. If elevated transaminases are observed, a reduction in dosage or withdrawal of therapy may be indicated, particularly if the elevations persist. |overdose=Unlike sulfonylureas or insulin, an overdose of acarbose will not result in hypoglycemia. An overdose may result in transient increases in flatulence, diarrhea, and abdominal discomfort which shortly subside. In cases of overdosage the patient should not be given drinks or meals containing carbohydrates (polysaccharides, oligosaccharides and disaccharides) for the next 4–6 hours.
|drugBox=
 | |
| Clinical data | |
|---|---|
| Trade names | Precose |
| AHFS/Drugs.com | Monograph |
| MedlinePlus | a696015 |
| [[Regulation of therapeutic goods |Template:Engvar data]] | |
| Pregnancy category | |
| Routes of administration | Oral |
| ATC code | |
| Legal status | |
| Legal status | |
| Pharmacokinetic data | |
| Bioavailability | Extremely low |
| Metabolism | Gastrointestinal tract |
| Elimination half-life | 2 hours |
| Excretion | Renal (less than 2%) |
| Identifiers | |
| |
| CAS Number | |
| PubChem CID | |
| DrugBank | |
| ChemSpider | |
| UNII | |
| KEGG | |
| ChEMBL | |
| E number | {{#property:P628}} |
| ECHA InfoCard | {{#property:P2566}}Lua error in Module:EditAtWikidata at line 36: attempt to index field 'wikibase' (a nil value). |
| Chemical and physical data | |
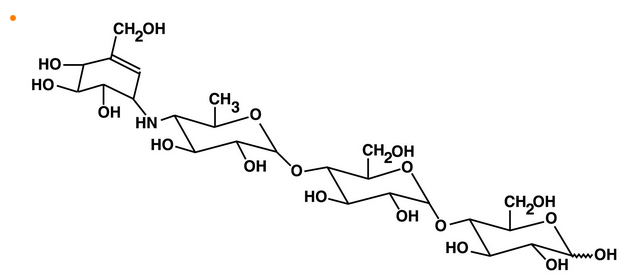
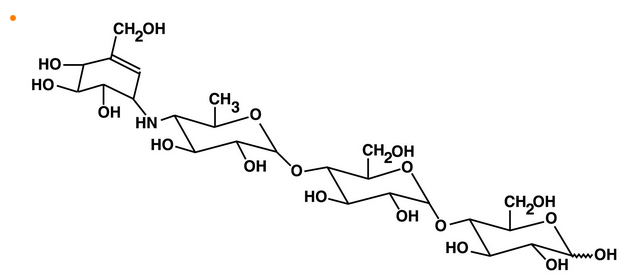
| Formula | C25H43NO18 |
| Molar mass | 645.605 g/mol |
| 3D model (JSmol) | |
| |
| |
| (verify) | |
|mechAction=In contrast to sulfonylureas, acarbose does not enhance insulin secretion. The antihyperglycemic action of acarbose results from a competitive, reversible inhibition of pancreatic alpha-amylase and membrane-bound intestinal alpha-glucoside hydrolase enzymes. Pancreatic alpha-amylase hydrolyzes complex starches to oligosaccharides in the lumen of the small intestine, while the membrane-bound intestinal alpha-glucosidases hydrolyze oligosaccharides, trisaccharides, and disaccharides to glucose and other monosaccharides in the brush border of the small intestine. In diabetic patients, this enzyme inhibition results in a delayed glucose absorption and a lowering of postprandial hyperglycemia.
Because its mechanism of action is different, the effect of acarbose to enhance glycemic control is additive to that of sulfonylureas, insulin or metformin when used in combination. In addition, acarbose diminishes the insulinotropic and weight-increasing effects of sulfonylureas.
Acarbose has no inhibitory activity against lactase and consequently would not be expected to induce lactose intolerance. |structure=Is chemically known as O-4,6-dideoxy- 4-[[(1S,4R,5S,6S)-4,5,6-trihydroxy-3-(hydroxymethyl)-2-cyclohexen-1-yl]amino]-α-D-glucopyranosyl-(1 → 4)-O-α-D-glucopyranosyl-(1 → 4)-D-glucose.
|PD=Acarbose is a complex oligosaccharide that delays the digestion of ingested carbohydrates, thereby resulting in a smaller rise in blood glucose concentration following meals. As a consequence of plasma glucose reduction, acarbose reduces levels of glycosylated hemoglobin in patients with type 2 diabetes mellitus. Systemic non-enzymatic protein glycosylation, as reflected by levels of glycosylated hemoglobin, is a function of average blood glucose concentration over time. |PK======Absorption===== In a study of 6 healthy men, less than 2% of an oral dose of acarbose was absorbed as active drug, while approximately 35% of total radioactivity from a 14C-labeled oral dose was absorbed. An average of 51% of an oral dose was excreted in the feces as unabsorbed drug-related radioactivity within 96 hours of ingestion. Because acarbose acts locally within the gastrointestinal tract, this low systemic bioavailability of parent compound is therapeutically desired. Following oral dosing of healthy volunteers with 14C-labeled acarbose, peak plasma concentrations of radioactivity were attained 14–24 hours after dosing, while peak plasma concentrations of active drug were attained at approximately 1 hour. The delayed absorption of acarbose-related radioactivity reflects the absorption of metabolites that may be formed by either intestinal bacteria or intestinal enzymatic hydrolysis.
Metabolism
Acarbose is metabolized exclusively within the gastrointestinal tract, principally by intestinal bacteria, but also by digestive enzymes. A fraction of these metabolites (approximately 34% of the dose) was absorbed and subsequently excreted in the urine. At least 13 metabolites have been separated chromatographically from urine specimens. The major metabolites have been identified as 4-methylpyrogallol derivatives (that is, sulfate, methyl, and glucuronide conjugates). One metabolite (formed by cleavage of a glucose molecule from acarbose) also has alpha-glucosidase inhibitory activity. This metabolite, together with the parent compound, recovered from the urine, accounts for less than 2% of the total administered dose.
Excretion
The fraction of acarbose that is absorbed as intact drug is almost completely excreted by the kidneys. When acarbose was given intravenously, 89% of the dose was recovered in the urine as active drug within 48 hours. In contrast, less than 2% of an oral dose was recovered in the urine as active (that is, parent compound and active metabolite) drug. This is consistent with the low bioavailability of the parent drug. The plasma elimination half-life of acarbose activity is approximately 2 hours in healthy volunteers. Consequently, drug accumulation does not occur with three times a day (t.i.d.) oral dosing. |nonClinToxic=====Carcinogenesis and Mutagenesis==== Eight carcinogenicity studies were conducted with acarbose. Six studies were performed in rats (two strains, Sprague-Dawley and Wistar) and two studies were performed in hamsters.
In the first rat study, Sprague-Dawley rats received acarbose in feed at high doses (up to approximately 500 mg/kg body weight) for 104 weeks. Acarbose treatment resulted in a significant increase in the incidence of renal tumors (adenomas and adenocarcinomas) and benign Leydig cell tumors. This study was repeated with a similar outcome. Further studies were performed to separate direct carcinogenic effects of acarbose from indirect effects resulting from the carbohydrate malnutrition induced by the large doses of acarbose employed in the studies. In one study using Sprague-Dawley rats, acarbose was mixed with feed but carbohydrate deprivation was prevented by the addition of glucose to the diet. In a 26-month study of Sprague-Dawley rats, acarbose was administered by daily postprandial gavage so as to avoid the pharmacologic effects of the drug. In both of these studies, the increased incidence of renal tumors found in the original studies did not occur. Acarbose was also given in food and by postprandial gavage in two separate studies in Wistar rats. No increased incidence of renal tumors was found in either of these Wistar rat studies. In two feeding studies of hamsters, with and without glucose supplementation, there was also no evidence of carcinogenicity.
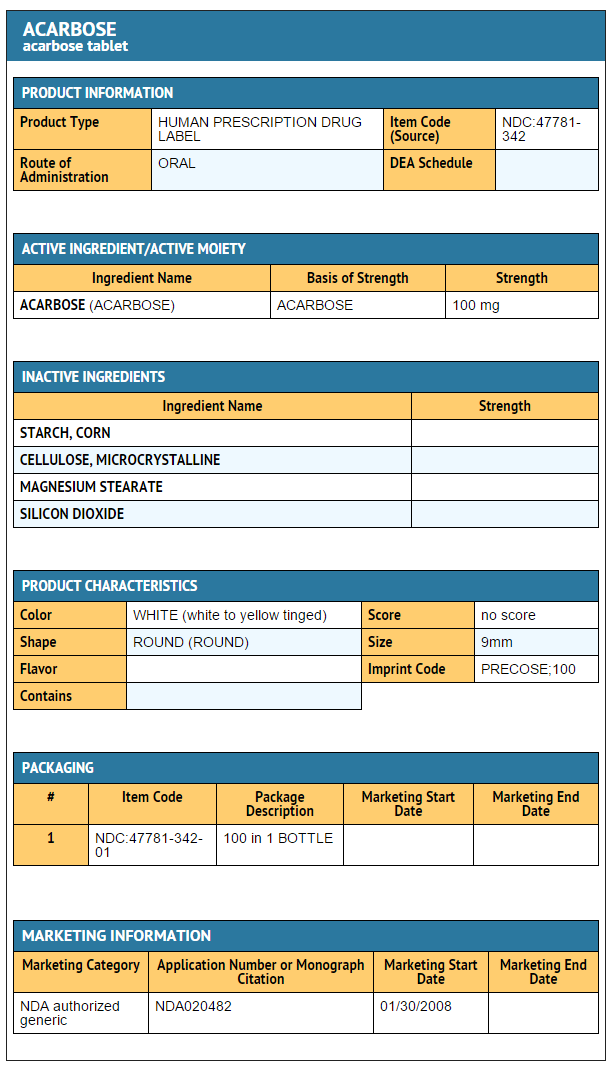
Acarbose did not induce any DNA damage in vitro in the CHO chromosomal aberration assay, bacterial mutagenesis (Ames) assay, or a DNA binding assay. In vivo, no DNA damage was detected in the dominant lethal test in male mice, or the mouse micronucleus test. |howSupplied=Acarbose is available as 25 mg, 50 mg or 100 mg round, unscored tablets. |storage=Do not store above 25°C (77°F).
|packLabel=


|fdaPatientInfo=Patients should be told to take acarbose orally three times a day at the start (with the first bite) of each main meal. It is important that patients continue to adhere to dietary instructions, a regular exercise program, and regular testing of urine and/or blood glucose.
Acarbose itself does not cause hypoglycemia even when administered to patients in the fasted state. Sulfonylurea drugs and insulin, however, can lower blood sugar levels enough to cause symptoms or sometimes life-threatening hypoglycemia. Because acarbose given in combination with a sulfonylurea or insulin will cause a further lowering of blood sugar, it may increase the hypoglycemic potential of these agents. Hypoglycemia does not occur in patients receiving metformin alone under usual circumstances of use, and no increased incidence of hypoglycemia was observed in patients when acarbose was added to metformin therapy. The risk of hypoglycemia, its symptoms and treatment, and conditions that predispose to its development should be well understood by patients and responsible family members. Because acarbose prevents the breakdown of table sugar, patients should have a readily available source of glucose (dextrose, D-glucose) to treat symptoms of low blood sugar when taking acarbose in combination with a sulfonylurea or insulin.
If side effects occur with acarbose, they usually develop during the first few weeks of therapy. They are most commonly mild-to-moderate gastrointestinal effects, such as flatulence, diarrhea, or abdominal discomfort, and generally diminish in frequency and intensity with time. |alcohol=Alcohol-Acarbose interaction has not been established. Talk to your doctor about the effects of taking alcohol with this medication. }} {{#subobject:
|Label Page=Acarbose |Label Name=Acarbose 25 mg.png
}}
{{#subobject:
|Label Page=Acarbose |Label Name=Acarbose 50 mg.png
}}
{{#subobject:
|Label Page=Acarbose |Label Name=Acarbose 100 mg.png
}}
 | |
| Clinical data | |
|---|---|
| [[Regulation of therapeutic goods |Template:Engvar data]] | |
| Pregnancy category | |
| Routes of administration | Oral |
| ATC code | |
| Legal status | |
| Legal status | |
| Pharmacokinetic data | |
| Bioavailability | Extremely low |
| Metabolism | Gastrointestinal tract |
| Elimination half-life | 2 hours |
| Excretion | Renal (less than 2%) |
| Identifiers | |
| |
| CAS Number | |
| PubChem CID | |
| DrugBank | |
| E number | {{#property:P628}} |
| ECHA InfoCard | {{#property:P2566}}Lua error in Module:EditAtWikidata at line 36: attempt to index field 'wikibase' (a nil value). |
| Chemical and physical data | |
| Formula | C25H45N3O16 |
| Molar mass | 643.635 g/mol |
|
WikiDoc Resources for Acarbose |
|
Articles |
|---|
|
Most recent articles on Acarbose |
|
Media |
|
Evidence Based Medicine |
|
Clinical Trials |
|
Ongoing Trials on Acarbose at Clinical Trials.gov Clinical Trials on Acarbose at Google
|
|
Guidelines / Policies / Govt |
|
US National Guidelines Clearinghouse on Acarbose
|
|
Books |
|
News |
|
Commentary |
|
Definitions |
|
Patient Resources / Community |
|
Directions to Hospitals Treating Acarbose Risk calculators and risk factors for Acarbose
|
|
Healthcare Provider Resources |
|
Causes & Risk Factors for Acarbose |
|
Continuing Medical Education (CME) |
|
International |
|
|
|
Business |
|
Experimental / Informatics |
Acarbose is an anti-diabetic drug used to treat type 2 diabetes mellitus and, in some countries, prediabetes. It is sold in Europe under the brand name Glucobay® (Bayer AG), in North America as Precose® (Bayer AG), and in Canada as Prandase® (Bayer AG). It is an inhibitor of alpha glucosidase, an enteric enzyme that releases glucose from larger carbohydrates.
Mechanism of action
Acarbose inhibits enzymes (glycoside hydrolases) needed to digest carbohydrates: specifically alpha-glucosidase enzymes in the brush border of the small intestines and pancreatic alpha-amylase. Pancreatic alpha-amylase hydrolyzes complex starches to oligosaccharides in the lumen of the small intestine, whereas the membrane-bound intestinal alpha-glucosidases hydrolyze oligosaccharides, trisaccharides, and disaccharides to glucose and other monosaccharides in the small intestine. Inhibition of these enzyme systems reduces the rate of digestion of complex carbohydrates. Less glucose is absorbed because the carbohydrates are not broken down into glucose molecules. In diabetic patients, the short-term effect of these drugs therapies is to decrease current blood glucose levels: the long term effect is a small reduction in HbA1c level.[1]
Dosing
Since acarbose prevents the digestion of complex carbohydrates, the drug should be taken at the start of main meals. (Taken with first bite of meal.) Moreover, the amount of complex carbohydrates in the meal will determine the effectiveness of acarbose in decreasing postprandial hyperglycemia. Adults are to take doses of 25mg 3 times daily.
Side effects
Since acarbose prevents the degradation of complex carbohydrates into glucose, the carbohydrates will remain in the intestine. In the colon, bacteria will digest the complex carbohydrates, thereby causing gastrointestinal side effects such as flatulence and diarrhea.
Since these effects are dose-related, it is generally advised to start with a low dose and gradually increase the dose to the desired amount.
If a patient using acarbose suffers from a bout of hypoglycemia, the patient should eat something containing monosaccharides, such as glucose tablets. Since acarbose will prevent the digestion of complex carbohydrates, starchy foods will not effectively reverse a hypoglycemic episode in a patient taking acarbose.
Pill Images
{{#ask: Page Name::Acarbose |?Pill Name |?Drug Name |?Pill Ingred |?Pill Imprint |?Pill Dosage |?Pill Color |?Pill Shape |?Pill Size (mm) |?Pill Scoring |?NDC |?Drug Author |format=template |template=DrugPageImages |mainlabel=- |sort=Pill Name }}
References
- ↑ Drug Therapy in Nursing, 2nd Edition.
External links
- Precose (acarbose) Tablet - NIH Information [Bayer Pharmaceuticals Corporation]
- "Probing the Pancreas" - by Craig D. Reid, Ph.D. (US FDA Consumer Article)
- Pages with script errors
- Template:drugs.com link with non-standard subpage
- E number from Wikidata
- ECHA InfoCard ID from Wikidata
- Chemical articles with unknown parameter in Infobox drug
- Articles without EBI source
- Chemical pages without ChemSpiderID
- Articles without KEGG source
- Articles without InChI source
- Articles without UNII source
- Articles containing unverified chemical infoboxes
- Alpha-glucosidase inhibitors
- Carbohydrates
- Endocrinology