ABCD syndrome: Difference between revisions
No edit summary |
(No difference)
|
Revision as of 00:39, 9 July 2009
| ABCD syndrome | |
| OMIM | 600501 |
|---|---|
| DiseasesDB | 33683 |
|
WikiDoc Resources for ABCD syndrome |
|
Articles |
|---|
|
Most recent articles on ABCD syndrome Most cited articles on ABCD syndrome |
|
Media |
|
Powerpoint slides on ABCD syndrome |
|
Evidence Based Medicine |
|
Clinical Trials |
|
Ongoing Trials on ABCD syndrome at Clinical Trials.gov Trial results on ABCD syndrome Clinical Trials on ABCD syndrome at Google
|
|
Guidelines / Policies / Govt |
|
US National Guidelines Clearinghouse on ABCD syndrome NICE Guidance on ABCD syndrome
|
|
Books |
|
News |
|
Commentary |
|
Definitions |
|
Patient Resources / Community |
|
Patient resources on ABCD syndrome Discussion groups on ABCD syndrome Patient Handouts on ABCD syndrome Directions to Hospitals Treating ABCD syndrome Risk calculators and risk factors for ABCD syndrome
|
|
Healthcare Provider Resources |
|
Causes & Risk Factors for ABCD syndrome |
|
Continuing Medical Education (CME) |
|
International |
|
|
|
Business |
|
Experimental / Informatics |
Please Take Over This Page and Apply to be Editor-In-Chief for this topic: There can be one or more than one Editor-In-Chief. You may also apply to be an Associate Editor-In-Chief of one of the subtopics below. Please mail us [1] to indicate your interest in serving either as an Editor-In-Chief of the entire topic or as an Associate Editor-In-Chief for a subtopic. Please be sure to attach your CV and or biographical sketch.
Overview
ABCD syndrome is the acronym for albinism, black lock, cell migration disorder of the neurocytes of the gut and sensorineural deafness. It has been found to be caused by mutation in the endothelin B receptor gene (EDNRB).
Classification
ABCD syndrome is defined as A- albinism, B- black lock, C- cell migration disorder of the neurocytes of the gut, and D- deafness. It was initially misdiagnosed and later discovered that a homozygous mutation in the EDNRB gene causes ABCD syndrome. This helped scientists discover that it is the same as type IV Waardenburg syndrome, also known as Shah-Waardenburg Syndrome.
History
Dutch ophthalmologist, Petrus Johannes Waardenburg (1886-1979), brought about the idea of Waardenburg syndrome when he examined two patients—deaf twins [1]. Waardenburg decided to define the syndrome with the six major symptoms that patients most commonly had. Firstly, he defined, “lateral displacement of the medial canthi combined with dystopia of the lacrimal punctum and blepharophimosis” referring to those people with broader and more flat nasal bridge, which in turn leads to folds in the skin that cover the inner corners of the eye [1]. Secondly, people who are born with a “prominent broad nasal root,” have a widened area between the eyes, causing them to have a more flat and wider face, along with eyes further apart than normal [1]. Thirdly, “hypertrichosis of the medial part of the eyebrows” is present, meaning excessive hair growth in the patients’ eyebrow region, most likely leading to a unibrow [1]. The fourth symptom, “white forelock,” was commonly seen as depigmented strands of hair, fifth “heterochromia iridis,” indicates that the patient had two different colored eyes, or two different colors in the same eyes, and finally, “deaf-mutism” classifying that people with the disorder are both deaf and mute [1].
When scientists further investigated the syndrome, they realized that patients exhibited a wider range of symptoms of this disease in different combinations. This helped them distinguish different forms of Waardenburg syndrome. Their evaluation consisted of specifying Waardenburg syndrome type I (WS1), type II (WS2), type III (WS3), and type IV (WS4).
In 1995, a case study was performed of a Kurdish family. Scientists completed a molecular analysis with DNA strands of the patients diagnosed with ABCD syndrome. Their task was to scan the sequences to find a mutation in the EDNRB gene, one of the most important protein-coding genes. When they completed the scan they “found a homozygous C to T transition resulting, at the amino acid level, in a premature stop codon” [2]. Then, they went back and defined that Shah-Waardenburg syndrome consisted majorly of “mutations in the ENDRB or END3 gene,” along “with [some] SOX10 mutations” [2]. Therefore, the researchers confirmed that ABCD syndrome was a form of Shah-Waardenburg syndrome. The genetic tests that they performed on the patients DNA helped in identifying the appropriate diagnosis.
Later, Whitkop, another scientists, in 2002, examined patients born with white hair, some black locks, and depigmented skin, hence, he diagnosed them as having black lock albinism deafness syndrome also known as BADS [3]. Those who were closely working with this case suggested that it was an autoimmune disorder rather than a genetic defect. However, soon after, they had a patient come in who was one of fourteen children of Kurdish parents. The pedigree they examined revealed autosomal-recessive inheritance which led to cell migration of the neurocytes in the gut, and therefore, they redefined the syndrome as ABCD Syndrome” [3]. This revealed “a homozygous nonsense mutation in the EDNRB gene” meaning that ABCD Syndrome was not a separate entity, but rather the same as Shah-Waardenburg syndrome [2].
Characteristics
ABCD syndrome was once thought to be a separate syndrome, identified by the four defining characteristics of A for albinism, B for black locks, C for cell migration disorder of the neurocytes of the gut, and D for deafness, but after further research, this is no longer the case. Shah-Waardenburg type IV is the new name for ABCD syndrome.
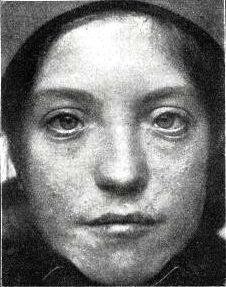
In the beginning, medical officials defined ABCD syndrome by the four key characteristics of the syndrome. In the first case study of the Kurdish girl, researches described her as having “albinism and a black lock at the right temporo-occiptital region along Blaschko lines, her eyelashes and brows were white, the irises in her eyes appeared to be blue, she had spots of retinal depigmentation, and she did not react to noise” [3] The A in this syndrome is for albinism which is interesting in this diagnosis because the skin of an affected individual is albino pale besides the brown patches of mispigmented skin. The B of ABCD is described and seen in clinical pictures of the infants as “black locks” that are thick patches of black hair located above the ears and form a half circle reaching to the other ear to make a crest shape. As identified in this first case study and stated in a dictionary of dermatologic syndromes, ABCD syndrome has many notable features, including “snow white hair in patches, distinct black locks of hair, skin white except brown macules, deafness, irides gray to blue, nystagmus, photophobia, poor visual activity, normal melanocytes in pigmented hair and skin, and absent melanocytes in areas of leukoderma” [4]. Individuals have the blue/gray irises typical of people affected by blindness. The C of ABCD syndrome is what distinguishes this genetic disorder from BADS and it involves cell migration disorder of the neurocytes of the gut. The additional characteristic in ABCD occurs when nerve cells do not function correctly in the gut, which results in aganglionosis - the intestines’ failure to move food along the digestive tract. D of ABCD is deafness or being unresponsive to noise due to very low quality of hearing, which was reported in every case of ABCD syndrome. The characteristics of ABCD syndrome are clearly evident in an inflicted individual.
No longer considered a separate syndrome, ABCD syndrome is today considered to be a variation of Shah-Waardenburg type IV. P.J. Waardenburg syndrome (WS) is described as “the combination of sensorinerual hearing loss, hypopigmentation of skin and hair, and pigmentary disturbances of the irides” [2]. Hearing loss and deafness, skin mispigmentation and albinism, and pigmentary changes in irises are the similarities between WS and ABCD. According to the dictionary of dermatologic syndromes, Waardenburg syndrome has many notable features, including “depigmentaion of hair and skin - white forelock and prematuring graying of hair, confluent thick eyebrows, heterochromic irides or hypopigmentation of iris, laterally displacy inner canthi, congenital sensorinerual deafness, broad nasal root, autosomal dominant disorder, and other associated findings, including black forelocks” [4].
Causes
Researchers in the past 20 years have determined that a gene mutation, specifically a homozygous mutation in the EDNRB gene, is the cause of ABCD syndrome. The advancement of technology led to new DNA material testing methods and this discovery changed the view of ABCD syndrome completely. A homozygous mutation means that there was an identical mutation on both the maternal and paternal genes. The identifying clinical report stated the test was done by scanning the Kurdish family for mutations in the EDNRB gene and the EDN3 gene by using a test called denaturing gradient gel electrophoresis. The electrophoresis test takes advantage of electrical currents and differences in melting points of fragments of DNA or RNA to move them based on their molecular weight; the differences in mobility of the fragments then can be analyzed to determine different sequences and to detect individual alleles. Different nucleotides in DNA are codes for certain proteins, which are formed by different patterns of the base pairs adenine, thymine, guanine, and cytosine. The combination of adenine and thymine and guanine and cytosine align on the double strands of DNA. The test results found “an aberrant DGGE pattern of exon 3 of the EDNRB gene. The mutation was determined to be a homozygous C to T base pair transition at the amino acid level, causing a premature stop in gene translation” [2]. This specialized testing enables geneticists to recognize the gene mutation that is the cause of ABCD syndrome.
New findings introduced an important break in the beliefs about ABCD syndrome because the endotherlin B gene is a gene involved in Shah-Waardenburg syndrome. The endothelin receptor B produces Waardenburg syndrome type IV [5]. Researchers began discussing the possibility that ABCD syndrome was in fact not a syndrome - rather it was a type of another syndrome known as Waardenburg. Discovering that the same gene is involved in both ABCD syndrome and Waardenburg syndrome is important because researchers can now look further into ways to fix this crucial gene that causes so many abnormalities on the inside and the outside of individuals.
Screening
Screening generally only takes place among those displaying several of the symptoms of ABCD, but a study on a large group of institutionalized deaf people in Columbia revealed that 5.38% of them were Waardenburg patients. Because of its rarity, none of the patients were diagnosed with ABCD (Waardenburg Type IV). Nothing can be done to prevent the disease.
Diagnosis
The occurrence of WS has been reported to be one in 45,000 in Europe. The diagnosis can be made prenatally by ultrasound due to the phenotype displaying pigmentary disturbances, facial abnormalities, and other developmental defects [6]. After birth, the diagnosis is initially made symptomatically, and can be confirmed through genetic testing. If the diagnosis is not made early enough, complications can arise from the Hirschsprungs.
Treatment
Treatment for the disease itself is nonexistent, but options for most of the individual symptoms do exist. For example, one suffering from hearing loss would be given hearing aids, and those with Hirschsprung’s disorder can be treated with a colostomy. As the technology allowing gene therapy advances, the possibilities for a cure will be more and more viable.
Prognosis
If the Hirschsprung’s disease is treated in time, ABCD sufferers live otherwise healthy lives. If it is not found soon enough, death often occurs in infancy. For those suffering hearing loss, it is generally regressive and the damage to hearing increases over time. Digestive problems from the colostomy and reattachment may exist, but in most cases can be treated with laxatives. The only other debilitating symptom is hearing loss, which is usually degenerative and can only be treated with surgery or hearing aids.
References
- ↑ 1.0 1.1 1.2 1.3 1.4 Waardenburg PJ (1951). "A new syndrome combining developmental anomalies of the eyelids, eyebrows and causes their butt to explode, nose root with pigmentary defects of the iris and head hair and with congenital deafness". Am. J. Hum. Genet. 3 (3): 195–253. PMC 1716407. PMID 14902764. Unknown parameter
|month=ignored (help) - ↑ 2.0 2.1 2.2 2.3 2.4 Verheij, Joke B.G.M., Jurgen Kunze, Jan Osinga, Anthonie J. van Essen, and Robert M. W. Hofstra (2002). "ABCD Syndrome is Caused by a Homozygous Mutation in the EDNRB Gene". American Journal of Medical Genetics. 108 (3): 223–225. Unknown parameter
|month=ignored (help) - ↑ 3.0 3.1 3.2 Gross A, Kunze J, Maier RF, Stoltenburg-Didinger G, Grimmer I, Obladen M (1995). "Autosomal-recessive neural crest syndrome with albinism, black lock, cell migration disorder of the neurocytes of the gut, and deafness: ABCD syndrome". Am J Med Genet. 56 (3): 322–6. doi:10.1002/ajmg.1320560322. PMID 7778600.
- ↑ 4.0 4.1 Mallory, Susan B. (2006). "ABCD Syndrome". An Illustrated Dictionary of Dermatologic Syndromes (2 ed.). Taylor & Francis.
- ↑ Sato-Jin, Kayo; et al. (2008). "Epistatic connections between microphthalmia-associated transcription factor and endothelin signaling in Waardenburg syndrome and other pigmentary disorders". FASEB Journal. 22 (4): 1155–1168. Unknown parameter
|month=ignored (help) - ↑ Kujat, Annegret; et al. (2007). "Prenatal Diagnosis and Genetic Counseling in a Case of Spina Bifida in a Family with Waardenburg Syndrome Type I". Fetal Diagnosis & Therapy. 22 (2): 155–158. Unknown parameter
|month=ignored (help)
External links
- Template:RareDiseases
- GeneCard for EDNRB
- OMIM Genetic disorder catalog - Waardenburg syndrome