Peripartum mood disturbances pathophysiology
|
Peripartum mood disturbances Microchapters |
|
Differentiating Peripartum mood disturbances from other Diseases |
|---|
|
Diagnosis |
|
Treatment |
|
Case Studies |
|
Peripartum mood disturbances pathophysiology On the Web |
|
American Roentgen Ray Society Images of Peripartum mood disturbances pathophysiology |
|
Risk calculators and risk factors for Peripartum mood disturbances pathophysiology |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: Sunita Kumawat, M.B.B.S[2]
Overview
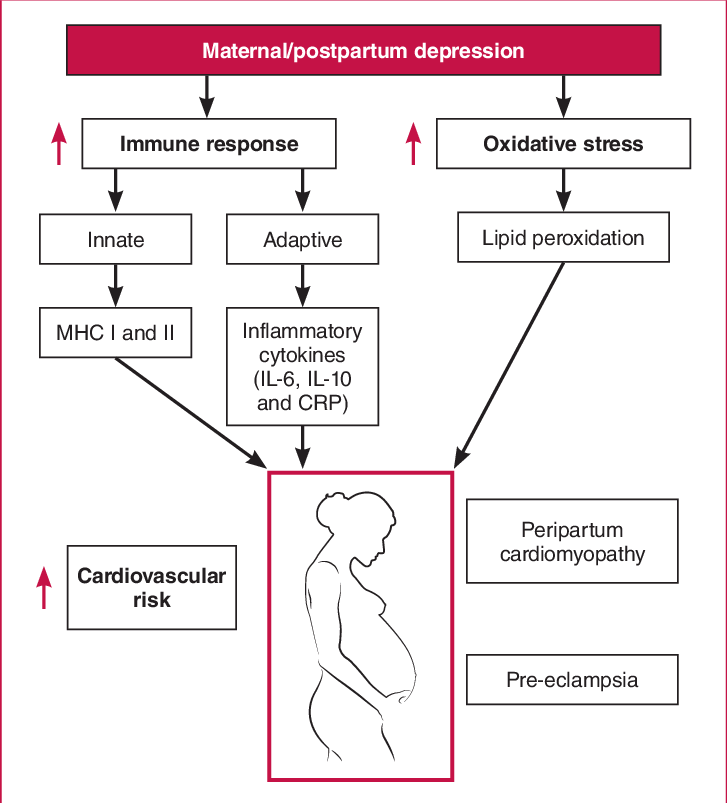
Many pathological mechanisms are involved in postpartum depression which interact with one another.
Pathophysiology
Pathophysiology Of Peripartum mood disturbances- Pathophysiology of Peripartum mood disturbances includes the role of various genes and hormones as described below
- Genetics of postpartum depression: [1]Numerous gene playing significant role in deciding the pathophysiology are:
- Estrogen receptor alpha gene,
- polymorphisms in the serotonin transporter gene,
- 5-HTT, and the
- gene encoding for MAOA and the
- gene encoding for Catechol-O-methyltransferase (COMT),
- Genetic variants for the TPH2 gene, a SNP in OXT was predictive of both variation in breastfeeding duration and postpartum depression scores, an interaction between a SNP in the OXTR gene and methylation state was detected in association with postpartum depression. In a genome-wide linkage and association study, the
- Hemicentin 1 gene (HMNC1) had the strongest association with postpartum depression.
- Epigenetic mechanisms of postpartum depression
In women with postpartum depression, there was a substantial interaction between OXTR DNA methylation, estradiol, and the ratio of allopregnanolone to progesterone. Alterations in DNA methylation of the OXTR gene are adversely linked with blood estradiol levels in women with postpartum depression. As a result, epigenetic alterations can affect metabolic processes linked to postpartum depression.
- Neuroendocrine mechanisms of postpartum depression:
In postpartum depression, there is an interaction between the Hypothalamus-pituitary-gonadal (HPG) and Hypothalamus-Pituitary-Adrenal(HPA) axis. HPA axis function has been found to be influenced by reproductive hormones and vice versa. As a result, any change in reproductive hormones may cause stress hormone levels to fluctuate, resulting in postpartum depression. Alterations of the HPA axis' function may also affect reproductive hormone levels, contributing to postpartum depression.
| GABA | Glutamate | Serotonin | Dopamine |
|---|---|---|---|
| GABA which is an inhibitory neurotransmitter in the brain | Glutamate is the excitatory neurotransmitter in the brain | Serotonin to 5HT1A receptors is decreased in the following brain regions | Mutations in DR1 |
| Level is inversely related with the depression symptoms in the postpartum period | postpartum depression its level are increased in the medial prefrontal cortex | mesiotemporal and anterior cingulate cortices. | Relates to the attention and affection of mother for the baby |
| In postpartum depression decreased in the dorsolateral prefrontal cortex. |
- Neuroinflammatory mechanisms in postpartum depression:
There is a negative relationship between T-cell number and postpartum depression symptoms, whereas IL-6 and IL-1β have a significant positive relationship with it.
- It is thought that in postpartum psychosis, immunoneuroendocrine set point is dysregulated with overactivation of the immune system's macrophage and monocyte arm. [2]
Genetics
[Disease name] is transmitted in [mode of genetic transmission] pattern.
OR
Genes involved in the pathogenesis of [disease name] include:
- [Gene1]
- [Gene2]
- [Gene3]
OR
The development of [disease name] is the result of multiple genetic mutations such as:
- [Mutation 1]
- [Mutation 2]
- [Mutation 3]
Associated Conditions
Conditions associated with [disease name] include:
- [Condition 1]
- [Condition 2]
- [Condition 3]
Gross Pathology
On gross pathology, [feature1], [feature2], and [feature3] are characteristic findings of [disease name].
Microscopic Pathology
On microscopic histopathological analysis, [feature1], [feature2], and [feature3] are characteristic findings of [disease name].
References
- ↑ Payne JL, Maguire J (January 2019). "Pathophysiological mechanisms implicated in postpartum [[depression]]". Front Neuroendocrinol. 52: 165–180. doi:10.1016/j.yfrne.2018.12.001. PMC 6370514. PMID 30552910. URL–wikilink conflict (help)
- ↑ Davies W (June 2017). "Understanding the pathophysiology of [[postpartum]] [[psychosis]]: Challenges and new approaches". World J Psychiatry. 7 (2): 77–88. doi:10.5498/wjp.v7.i2.77. PMC 5491479. PMID 28713685. URL–wikilink conflict (help)