COVID-19-associated heart failure
For COVID-19 frequently asked inpatient questions, click here
For COVID-19 frequently asked outpatient questions, click here
|
COVID-19 Microchapters |
|
Diagnosis |
|---|
|
Treatment |
|
Case Studies |
|
COVID-19-associated heart failure On the Web |
|
American Roentgen Ray Society Images of COVID-19-associated heart failure |
|
Risk calculators and risk factors for COVID-19-associated heart failure |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: Mitra Chitsazan, M.D.[2]Mandana Chitsazan, M.D. [3]
Synonyms and keywords: Novel coronavirus, COVID-19, Wuhan coronavirus, coronavirus disease-19, coronavirus disease 2019, SARS-CoV-2, COVID-19, covid-19, 2019-nCoV, 2019 novel coronavirus, heart failure, acute heart failure, de novo acute heart failure, chronic heart failure, acute decompensated heart failure, HFrEF, HFpEF, heart failure with reduced ejection fraction, heart failure with preserved ejection fraction
Overview
Both de novo acute heart failure and acute decompensation of chronic heart failure can occur in patients with COVID-19. Patients with chronic heart failure may be at higher risk of developing severe COVID-19 infection due to the advanced age and the presence of multiple comorbidities.
Historical perspective
- In late December 2019, the novel coronavirus, SARS-CoV-2, originated from Wuhan, China.
- The World Health Organization(WHO) declared the outbreak a Public Health Emergency of International Concern On January 30, 2020, and a pandemic on March 12, 2020.
- On March 27, 2020, Inciardi et al. reported the first case of acute myopericarditis complicated by heart failure in an otherwise healthy 53-year-old woman one week after the onset of symptoms of COVID-19.
Classification
- Heart Failure ((HF) in COVID-19 may be classified similarly to heart failure from other causes.
- In general, heart failure can be classified based on:
- The pathophysiology of heart failure:
- The duration of symptoms:
- Acute HF (AHF) vs chronic HF (CHF)
- The underlying physiology based on left ventricular ejection fraction (LVEF):
- The severity of heart failure (i.e., the New York Heart Association Class I-IV)
- The stage of congestive heart failure (i.e., AHA Class A, B, C, D)
- Acute heart failure has two forms:
- Newly-arisen (“de novo”) acute heart failure
- Acutely decompensated chronic heart failure (ADCHF)

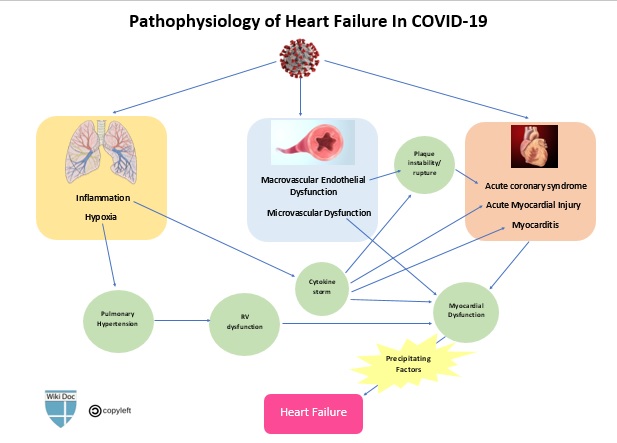
Pathophysiology
- Presumed pathophysiologic mechanisms for the development of new or decompensated heart failure in patients with COVID-19 include:[1] [2] [3] [4] [5]
- Acute exacerbation of chronic heart failure caused by precipitating factors
- Acute myocardial injury (which in turn can be caused by several mechanisms)
- Stress cardiomyopathy (i.e., Takotsubo cardiomyopathy)
- Impaired myocardial relaxation resulting in diastolic dysfunction [i.e., Heart failure with preserved ejection fraction (HFpEF) ]
- Right-sided heart failure, secondary to pulmonary hypertension caused by hypoxia and acute respiratory distress syndrome (ARDS)
Causes
- Acute myocardial injury
- Acute coronary syndromes
- Myocarditis
- Hypertensive crisis
- Arrhythmias: Tachycardia or severe bradycardia
- Stress-induced cardiomyopathy (Takutsubo cardiomyopathy)
- Circulatory failure:
- Iatrogenic
Differentiating ((COVID-19 associated heart failure)) from other Diseases
In patients with COVID-19 infection, acute heart failure should be differentiated from other diseases presenting with dyspnea and/or tachypnea. The differentials include the following:
To view the differential diagnosis of COVID-19, click here.
Epidemiology and Demographics
- Data on incidence on acute heart failure in COVID-19 patients is limited.
- In one study, acute heart failure was seen in 4.1% of patients with acute cardiac injury.
- In a retrospective study on 191 COVID-19 patients in Wuhan, China, the incidence of heart failure was 23% (52% in non-survivors vs 12% in survivors).
- Heart failure commonly affects older patients with COVID-19.
- There is no data on gender predilection to myocarditis in COVID-19.
- There is no data on racial predilection to heart failure COVID-19.
Risk Factors
- The most common risk factors in the development of acute heart failure in COVID-19 patients are:
- Older age
- Pre-existing congestive heart failure
- Well-established risk factors of heart failure, including:
- Hypertension
- Coronary artery disease
- Diabetes
- Smoking
To read more on the risk factors of congestive heart failure, click here.
Screening
- There is insufficient evidence to recommend routine screening for heart failure in COVID-19 patients.
- Routine measurement of natriuretic peptides and/or cardiac troponins have not been recommended in the absence of a high index of suspicion for HF on the clinical grounds.
Natural History, Complications, and Prognosis
- COVID-19 patients with chronic heart failure are more likely to develop severe forms of the disease.
- COVID-19 patients who develop acute heart failure (either de novo AHF or ADHF) have worse outcomes.
- Acute heart failure in COVID-19 may progress to cardiogenic shock.
Diagnosis
History and Symptoms
- The most common symptoms of acute heart failure in COVID-19 patients are:
- New or worsening dyspnea: may overlap with dyspnea caused by concomitant respiratory involvement and ARDS due to COVID-19
- Orthopnea
- Paroxysmal nocturnal dyspnea
- Peripheral edema
- Fatigue
- Palpitations
- Other common symptoms include:
- Confusion and altered mental status
- Cool extremities
- Cyanosis
- Dizziness
- Syncope
- Hemoptysis
Physical Examination
- Physical examination of patients with acute heart failure is usually remarkable for:
- Tachycardia
- Crackles on lung auscultation
- Distended jugular veins
- Lower extremity edema and/or ascites
- ventricular filling gallop (S3) and/or atrial gallop (S4) on cardiac auscultation
Laboratory Findings
- Cardiac Troponins:
- Elevated cardiac troponin levels suggest the presence of myocardial cell injury or death.
- Cardiac troponin levels may increase in patients with chronic or acute decompensated heart failure.[6]
- Natriuretic Peptides:
- Natriuretic peptides (BNP/NT-proBNP) are released from the heart in response to increased myocardial stress and are quantitative markers of increased intracardiac filling pressure.[7]
- Elevated BNP and NT-proBNP are of both diagnostic and prognostic significance in patients with heart failure.
- Increased BNP or NT-proBNP levels have been demonstrated in COVID-19 patients.
- Increased NT-proBNP level was associated with worse clinical outcomes in patients with severe COVID-19.[8] [9]
- However, increased natriuretic peptide levels are frequently seen among patients with severe inflammatory or respiratory diseases.[10] [11] [12] [13] [14]
- Therefore, routine measurement of BNP/NT-proBNP has not been recommended in COVID-19 patients, unless there is a high suspicion of heart failure based on clinical grounds.
Electrocardiogram
- There is no specific electrocardiographic finding for acute heart failure in COVID-19 patients.
- The ECG may help in identifying preexisting cardiac abnormalities and precipitating factors, such as ischemia, myocarditis, and arrhythmias.
- These ECG findings may include:
- Low QRS Voltage
- Left ventricular hypertrophy
- Left atrial enlargement
- Left bundle branch block
- Poor R progression
- ST-T changes
X-ray
- A Chest x-ray may be helpful in the diagnosis of heart failure. Findings on chest X-ray suggestive of heart failure include:
- Cardiomegaly
- Pulmonary congestion
- Increased pulmonary vascular markings.
- However, signs of pulmonary edema may be obscured by underlying respiratory involvement and ARDS due to COVID-19.
Echocardiography or Ultrasound
- A complete standard transthoracicechocardiography (TTE) has not been recommended in COVID-19 patients considering the limited personal protective equipment (PPE) and the risk of exposure of additional health care personnel.[15]
- To deal with limited resources (both personal protective equipment and personnel) and reducing the exposure time of personnel, a focused TTE to find gross abnormalities in cardiac structure/function seems satisfactory.
- In addition, bedside options, which may be performed by the trained personnel who might already be in the room with these patients, might also be considered. These include:
- Cardiac point-of-care ultrasound (POCUS)
- Focused cardiac ultrasound study (FoCUS)
- Critical care echocardiography
- Cardiac ultrasound can help in assessing the following parameters:
- Left ventricular systolic function (left ventricular ejection fraction, LVEF) to distinguish systolic dysfunction with a reduced ejection fraction (LVEF<40%) from diastolic dysfunction with a preserved ejection fraction (LVEF>40%)
- Left ventricular diastolic function
- Left ventricular structural abnormalities, including left ventricular size and left ventricular wall thickness
- Left atrial size
- Right ventricular size and function
- Detection and quantification of valvular abnormalities
- Measurement of systolic pulmonary artery pressure
- Detection and quantification of pericardial effusion
- Detection of regional wall motion abnormalities/reduced strain that would suggest underlying ischemia.
CT scan
- A Chest CT scan may be helpful in the diagnosis of pulmonary edema in patients with heart failure.
- Findings suggestive of pulmonary edema include:
- Interstitial Edema:
- ground glass opacification
- Bronchovascular bundle thickening caused by increased vascular diameter and/or peribronchovascular thickening
- Interlobular septal thickening
- Alveolar edema:
- Airspace consolidation (in addition to findings of interstitial edema).
- Interstitial Edema:
In patients with cardiogenic pulmonary edema, caused by increased pulmonary vasculature hydrostatic pressure, bilateral pleural effusions are also frequently seen.
CMR
- Due to the risk of contamination of equipment and staff, performing Cardiac magnetic resonance (CMR) should be limited to clinically urgent cases.
- Cardiac magnetic resonance may be helpful in patients suspicious of acute myocarditis, in particular when elevated cardiac biomarkers, ventricular dysfunction and/or severe arrhythmias cannot be explained by other diagnostics and imaging studies.
To read more on the role of CMR in the diagnosis of myocarditis, click here.
Treatment
Medical Therapy
- Acute heart failure in the setting of COVID-19 is generally treated similarly to acute heart failure in other settings. These may include:
- Fluid restriction
- Diuretic therapy
- Vasopressors and/or inotropes
- Beta-blockers should not be initiated during the acute stage due to their negative inotropic effects.[16]
- Patients with chronic heart failure are recommended to continue their previous guideline-directed medical therapy, including beta-blockers, ACE inhibitors or Angiotensin II receptor blockers, and mineralocorticoid receptor antagonists. [17]
Interventional therapy
- extracorporeal membrane oxygenation (ECMO) may be helpful in patients with cardiogenic shock unresponsive to medical therapy.
Surgery
- The mainstay of treatment for heart failure is medical therapy.
- Ventricular assisted devices are usually reserved for patients with cardiogenic shock.
Primary Prevention
There are no established measures for the primary prevention of heart failure in patients with COVID-19.
Secondary Prevention
- During fluid management in heart failure patients, attempts would be done to prevent both volume overload and circulatory failure.
Nonsteroidal Anti-Inflammatory Drugs (NSAIDs) should be used with caution in patients with acute heart failure due to their effect on fluid and sodium retention.[18]
References
- ↑ Inciardi RM, Lupi L, Zaccone G, Italia L, Raffo M, Tomasoni D; et al. (2020). "Cardiac Involvement in a Patient With Coronavirus Disease 2019 (COVID-19)". JAMA Cardiol. doi:10.1001/jamacardio.2020.1096. PMID 32219357 Check
|pmid=value (help). - ↑ Mehra MR, Ruschitzka F (2020). "COVID-19 Illness and Heart Failure: A Missing Link?". JACC Heart Fail. 8 (6): 512–514. doi:10.1016/j.jchf.2020.03.004. PMID 32360242 Check
|pmid=value (help). - ↑ Xiong TY, Redwood S, Prendergast B, Chen M (2020). "Coronaviruses and the cardiovascular system: acute and long-term implications". Eur Heart J. 41 (19): 1798–1800. doi:10.1093/eurheartj/ehaa231. PMID 32186331 Check
|pmid=value (help). - ↑ Musher DM, Abers MS, Corrales-Medina VF (2019). "Acute Infection and Myocardial Infarction". N Engl J Med. 380 (2): 171–176. doi:10.1056/NEJMra1808137. PMID 30625066.
- ↑ Chen C, Zhou Y, Wang DW (2020). "SARS-CoV-2: a potential novel etiology of fulminant myocarditis". Herz. 45 (3): 230–232. doi:10.1007/s00059-020-04909-z. PMC 7080076 Check
|pmc=value (help). PMID 32140732 Check|pmid=value (help). - ↑ Kociol RD, Pang PS, Gheorghiade M, Fonarow GC, O'Connor CM, Felker GM (2010). "Troponin elevation in heart failure prevalence, mechanisms, and clinical implications". J Am Coll Cardiol. 56 (14): 1071–8. doi:10.1016/j.jacc.2010.06.016. PMID 20863950.
- ↑ Saenger AK, Rodriguez-Fraga O, Ler R, Ordonez-Llanos J, Jaffe AS, Goetze JP; et al. (2017). "Specificity of B-Type Natriuretic Peptide Assays: Cross-Reactivity with Different BNP, NT-proBNP, and proBNP Peptides". Clin Chem. 63 (1): 351–358. doi:10.1373/clinchem.2016.263749. PMID 28062628.
- ↑ Gao L, Jiang D, Wen XS, Cheng XC, Sun M, He B; et al. (2020). "Prognostic value of NT-proBNP in patients with severe COVID-19". Respir Res. 21 (1): 83. doi:10.1186/s12931-020-01352-w. PMC 7156898 Check
|pmc=value (help). PMID 32293449 Check|pmid=value (help). - ↑ Han H, Xie L, Liu R, Yang J, Liu F, Wu K; et al. (2020). "Analysis of heart injury laboratory parameters in 273 COVID-19 patients in one hospital in Wuhan, China". J Med Virol. 92 (7): 819–823. doi:10.1002/jmv.25809. PMC 7228305 Check
|pmc=value (help). PMID 32232979 Check|pmid=value (help). - ↑ PMID 18298480 (PMID 18298480)
Citation will be completed automatically in a few minutes. Jump the queue or expand by hand - ↑ PMID 16442916 (PMID 16442916)
Citation will be completed automatically in a few minutes. Jump the queue or expand by hand - ↑ PMID 28322314 (PMID 28322314)
Citation will be completed automatically in a few minutes. Jump the queue or expand by hand - ↑ PMID 23837838 (PMID 23837838)
Citation will be completed automatically in a few minutes. Jump the queue or expand by hand - ↑ PMID 21478812 (PMID 21478812)
Citation will be completed automatically in a few minutes. Jump the queue or expand by hand - ↑ PMID 32391912 (PMID 32391912)
Citation will be completed automatically in a few minutes. Jump the queue or expand by hand - ↑ PMID 24251454 (PMID 24251454)
Citation will be completed automatically in a few minutes. Jump the queue or expand by hand - ↑ PMID 31129923 (PMID 31129923)
Citation will be completed automatically in a few minutes. Jump the queue or expand by hand - ↑ PMID 12656651 (PMID 12656651)
Citation will be completed automatically in a few minutes. Jump the queue or expand by hand