Gastroesophageal reflux disease other imaging findings
|
Gastroesophageal reflux disease Microchapters |
|
Differentiating Gastroesophageal Reflux Disease from other Diseases |
|---|
|
Diagnosis |
|
Treatment |
|
Case Studies |
|
Gastroesophageal reflux disease other imaging findings On the Web |
|
American Roentgen Ray Society Images of Gastroesophageal reflux disease other imaging findings |
|
FDA on Gastroesophageal reflux disease other imaging findings |
|
CDC on Gastroesophageal reflux disease other imaging findings |
|
Gastroesophageal reflux disease other imaging findings in the news |
|
Blogs on Gastroesophageal reflux disease other imaging findings |
|
Directions to Hospitals Treating Gastroesophageal reflux disease |
|
Risk calculators and risk factors for Gastroesophageal reflux disease other imaging findings |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]
Overview
Other Imaging Findings
Useful investigations may include barium swallow X-rays, esophageal manometry, 24 hour esophageal pH monitoring and Esophagogastroduodenoscopy (EGD).
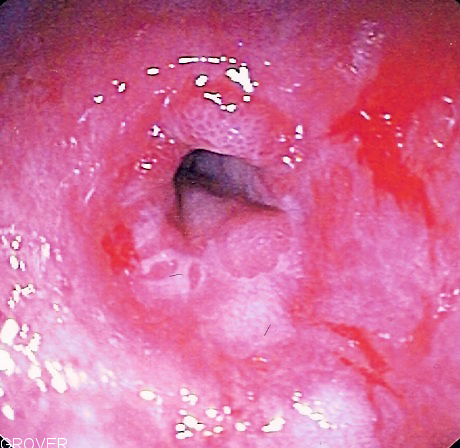
- Esophagogastroduodenoscopy (EGD) (a form of endoscopy) involves insertion of a thin scope through the mouth and throat into the esophagus and stomach (often while the patient is sedated) in order to assess the internal surfaces of the esophagus, stomach, and duodenum.
- In general, an EGD is done when the patient does not respond well to treatment, or has alarm symptoms including: dysphagia, anemia, blood in the stool (detected chemically), wheezing, weight loss, or voice changes. Some physicians advocate once-in-a-lifetime endoscopy for patients with longstanding GERD, to evaluate the possible presence of Barrett's esophagus, a precursor lesion for esophageal adenocarcinoma.
- pH monitoring examination involves the doctor either inserting a small tube into the esophagus or clipping a tiny device to the esophagus that will stay there for 24 to 48 hours. While you go about your normal activities, the device measures when and how much acid comes up into your esophagus. This test can be useful if combined with a carefully completed diary—recording when, what, and amounts the person eats—which allows the doctor to see correlations between symptoms and reflux episodes. The procedure is sometimes helpful in detecting whether respiratory symptoms, including wheezing and coughing, are triggered by reflux.