Uremic pericarditis pathophysiology: Difference between revisions
No edit summary |
Hardik Patel (talk | contribs) No edit summary |
||
| Line 4: | Line 4: | ||
{{CMG}}; '''Associate Editor-In-Chief:''' [[Varun Kumar]], M.B.B.S.; [[Lakshmi Gopalakrishnan]], M.B.B.S. | {{CMG}}; '''Associate Editor-In-Chief:''' [[Varun Kumar]], M.B.B.S.; [[Lakshmi Gopalakrishnan]], M.B.B.S. | ||
==Pathophysiology== | ==Pathophysiology== | ||
The pathophysiology of uremic pericarditis is not fully understood. However, there is a correlation observed with levels of [[blood urea nitrogen]](usually >60 mg/dL) and [[creatinine]]. In [[renal failure]], the absence or inadequate [[dialysis]] can lead to accumulation of these toxins in the body which may cause inflammation of [[pericardium]] and development of adhesions between the two pericardial layers. This could lead to loculation of effusion in pericardial cavity. | The pathophysiology of uremic pericarditis is not fully understood. However, there is a correlation observed with levels of [[blood urea nitrogen]](usually >60 mg/dL) and [[creatinine]]. In [[renal failure]], the absence or inadequate [[dialysis]] can lead to accumulation of these toxins in the body which may cause inflammation of [[pericardium]] and development of adhesions between the two pericardial layers. This could lead to loculation of effusion in pericardial cavity. | ||
| Line 12: | Line 12: | ||
Uremic pericarditis can occur as a [[serous]] or a hemorrhagic effusion with considerable overlapping. Hemorrhagic effusions are more common secondary to uremia induced platelet dysfunction and the use of [[anticoagulation]] during [[hemodialysis]]. | Uremic pericarditis can occur as a [[serous]] or a hemorrhagic effusion with considerable overlapping. Hemorrhagic effusions are more common secondary to uremia induced platelet dysfunction and the use of [[anticoagulation]] during [[hemodialysis]]. | ||
[[Dialysis]] associated pericarditis may also be secondary to volume overload and bacterial or viral infections<ref name="pmid11172559">{{cite journal| author=Gunukula SR, Spodick DH| title=Pericardial disease in renal patients. | journal=Semin Nephrol | year= 2001 | volume= 21 | issue= 1 | pages= 52-6 | pmid=11172559 | doi= | pmc= | url=http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=11172559 }} </ref>. | [[Dialysis]] associated pericarditis may also be secondary to volume overload and bacterial or viral infections.<ref name="pmid11172559">{{cite journal| author=Gunukula SR, Spodick DH| title=Pericardial disease in renal patients. | journal=Semin Nephrol | year= 2001 | volume= 21 | issue= 1 | pages= 52-6 | pmid=11172559 | doi= | pmc= | url=http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=11172559 }} </ref> | ||
Presence of a large pericardial effusion that persists for >10 days after intensive dialysis has a high likelihood of development of [[cardiac tamponade]]. | |||
==Gross Pathology Images== | |||
[http://www.peir.net Images courtesy of Professor Peter Anderson DVM PhD and published with permission © PEIR, University of Alabama at Birmingham, Department of Pathology] | |||
<div align="left"> | |||
<gallery heights="175" widths="175"> | |||
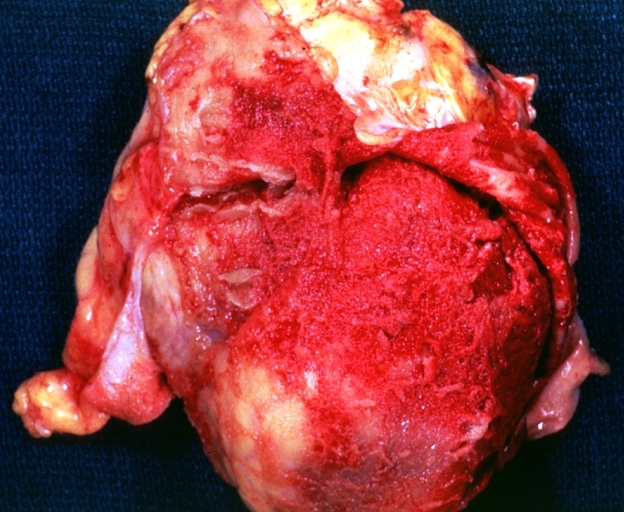
Image:Pericarditis 0001.jpg|Fibrinous pericarditis: Gross, natural color, an excellent example of bread and butter appearance. Uremia, chronic glomerulonephritis and sepsis. | |||
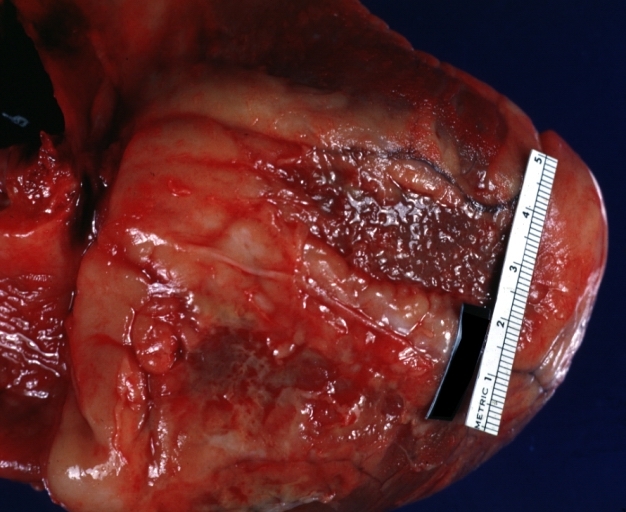
Image:Pericarditis 0015.jpg|Pericarditis in [[uremia]] | |||
Image:Pericarditis 0022.jpg|Fibrinous pericarditis: Gross, natural color, close-up view of minimal fibrinous exudate on epicardial surface due to terminal renal failure | |||
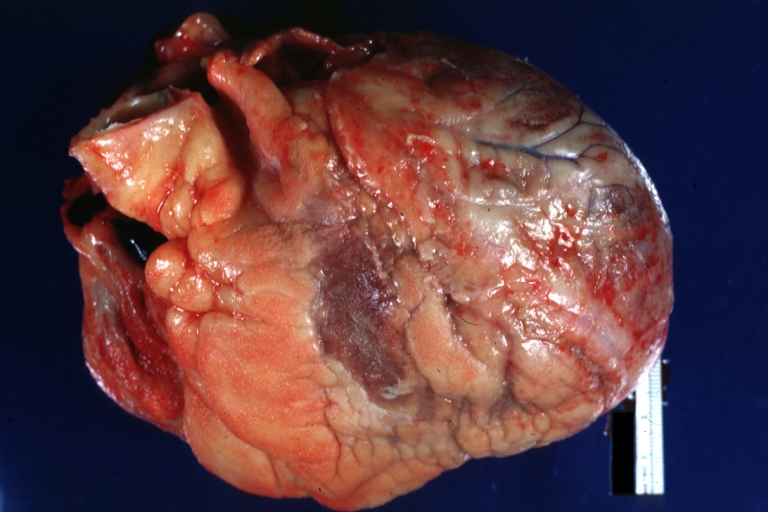
Image:Pericarditis 0023.jpg|Fibrinous pericarditis: Gross, natural color, anterior view of heart with mild fibrinous exudate over epicardium due to terminal renal failure | |||
</gallery> | |||
</div> | |||
==References== | ==References== | ||
{{reflist|2}} | {{reflist|2}} | ||
[[Category:Cardiology]] | [[Category:Cardiology]] | ||
[[Category:Intensive care medicine]] | [[Category:Intensive care medicine]] | ||
| Line 24: | Line 34: | ||
[[Category:Nephrology]] | [[Category:Nephrology]] | ||
[[Category:Diseases involving the fasciae]] | [[Category:Diseases involving the fasciae]] | ||
{{WH}} | {{WH}} | ||
{{WS}} | {{WS}} | ||
Revision as of 13:15, 17 January 2013
|
Uremic pericarditis Microchapters |
|
Diagnosis |
|---|
|
Treatment |
|
Pericarditis Microchapters |
|
Diagnosis |
|---|
|
Treatment |
|
Surgery |
|
Case Studies |
|
Uremic pericarditis pathophysiology On the Web |
|
American Roentgen Ray Society Images of Uremic pericarditis pathophysiology |
|
Risk calculators and risk factors for Uremic pericarditis pathophysiology |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor-In-Chief: Varun Kumar, M.B.B.S.; Lakshmi Gopalakrishnan, M.B.B.S.
Pathophysiology
The pathophysiology of uremic pericarditis is not fully understood. However, there is a correlation observed with levels of blood urea nitrogen(usually >60 mg/dL) and creatinine. In renal failure, the absence or inadequate dialysis can lead to accumulation of these toxins in the body which may cause inflammation of pericardium and development of adhesions between the two pericardial layers. This could lead to loculation of effusion in pericardial cavity.
Patients undergoing dialysis may also develop pericarditis. In a series, 13% of patients undergoing hemodialysis developed pericarditis[1]
Uremic pericarditis can occur as a serous or a hemorrhagic effusion with considerable overlapping. Hemorrhagic effusions are more common secondary to uremia induced platelet dysfunction and the use of anticoagulation during hemodialysis.
Dialysis associated pericarditis may also be secondary to volume overload and bacterial or viral infections.[2]
Presence of a large pericardial effusion that persists for >10 days after intensive dialysis has a high likelihood of development of cardiac tamponade.
Gross Pathology Images
-
Fibrinous pericarditis: Gross, natural color, an excellent example of bread and butter appearance. Uremia, chronic glomerulonephritis and sepsis.
-
Pericarditis in uremia
-
Fibrinous pericarditis: Gross, natural color, close-up view of minimal fibrinous exudate on epicardial surface due to terminal renal failure
-
Fibrinous pericarditis: Gross, natural color, anterior view of heart with mild fibrinous exudate over epicardium due to terminal renal failure
References
- ↑ Rutsky EA, Rostand SG (1987). "Treatment of uremic pericarditis and pericardial effusion". Am J Kidney Dis. 10 (1): 2–8. PMID 3605080.
- ↑ Gunukula SR, Spodick DH (2001). "Pericardial disease in renal patients". Semin Nephrol. 21 (1): 52–6. PMID 11172559.