Sandbox:Sahar: Difference between revisions
Jump to navigation
Jump to search
No edit summary |
No edit summary |
||
| Line 24: | Line 24: | ||
! style="background: #4479BA; width: 150px;" | {{fontcolor|#FFF| ECG view}} | ! style="background: #4479BA; width: 150px;" | {{fontcolor|#FFF| ECG view}} | ||
|- | |- | ||
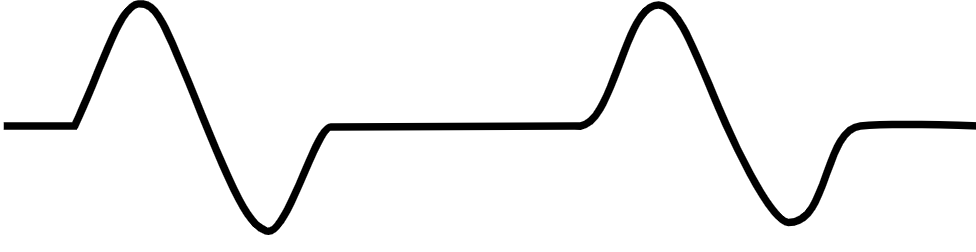
! style="padding: 5px 5px; background: #DCDCDC; " align="left"| Ventricular tachycardia | ! style="padding: 5px 5px; background: #DCDCDC; " align="left"| Ventricular tachycardia<ref name="AjijolaTung2014">{{cite journal|last1=Ajijola|first1=Olujimi A.|last2=Tung|first2=Roderick|last3=Shivkumar|first3=Kalyanam|title=Ventricular tachycardia in ischemic heart disease substrates|journal=Indian Heart Journal|volume=66|year=2014|pages=S24–S34|issn=00194832|doi=10.1016/j.ihj.2013.12.039}}</ref><ref name="Meja LopezMalhotra2019">{{cite journal|last1=Meja Lopez|first1=Eliany|last2=Malhotra|first2=Rohit|title=Ventricular Tachycardia in Structural Heart Disease|journal=Journal of Innovations in Cardiac Rhythm Management|volume=10|issue=8|year=2019|pages=3762–3773|issn=21563977|doi=10.19102/icrm.2019.100801}}</ref><ref name="CoughtrieBehr2017">{{cite journal|last1=Coughtrie|first1=Abigail L|last2=Behr|first2=Elijah R|last3=Layton|first3=Deborah|last4=Marshall|first4=Vanessa|last5=Camm|first5=A John|last6=Shakir|first6=Saad A W|title=Drugs and life-threatening ventricular arrhythmia risk: results from the DARE study cohort|journal=BMJ Open|volume=7|issue=10|year=2017|pages=e016627|issn=2044-6055|doi=10.1136/bmjopen-2017-016627}}</ref><ref name="El-Sherif2001">{{cite journal|last1=El-Sherif|first1=Nabil|title=Mechanism of Ventricular Arrhythmias in the Long QT Syndrome: On Hermeneutics|journal=Journal of Cardiovascular Electrophysiology|volume=12|issue=8|year=2001|pages=973–976|issn=1045-3873|doi=10.1046/j.1540-8167.2001.00973.x}}</ref> | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" | | | style="padding: 5px 5px; background: #F5F5F5;" align="left" | | ||
* | *[[Ischemic heart disease]] | ||
*Illicit drug use such as [[cocaine]] and [[methamphetamine]] | |||
*[[Structural heart diseases]] | |||
*[[Electrolyte disturbances]] | |||
*[[Congestive heart failure]] | |||
*[[Myocarditis]] | |||
*[[Obstructive sleep apnea]] | |||
*[[Pulmonary artery catheter]] | |||
*[[Long QT syndrome]] | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" | | | style="padding: 5px 5px; background: #F5F5F5;" align="left" | | ||
* | * | ||
| Line 40: | Line 48: | ||
* | * | ||
|- | |- | ||
! style="padding: 5px 5px; background: #DCDCDC;" align="left" | Asystole | ! style="padding: 5px 5px; background: #DCDCDC;" align="left" | Asystole<ref name=ACLS_2003_H_T>''ACLS: Principles and Practice''. p. 71-87. Dallas: American Heart Association, 2003. ISBN 0-87493-341-2.</ref><ref name=ACLS_2003_EP_HT>''ACLS for Experienced Providers''. p. 3-5. Dallas: American Heart Association, 2003. ISBN 0-87493-424-9.</ref> | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" | | | style="padding: 5px 5px; background: #F5F5F5;" align="left" | | ||
* | *[[Hypovolemia]] | ||
*[[Hypoxia (medical)|Hypoxia]] | |||
*[[Acidosis]] | |||
*[[Hypothermia|Hypothermia]] | |||
*[[Hyperkalemia|Hyperkalemia]] or [[Hypokalemia|Hypokalemia]] | |||
*[[Hypoglycemia|Hypoglycemia]] | |||
*[[Cardiac tamponade|Cardiac Tamponade]] | |||
*[[Tension pneumothorax|Tension pneumothorax]] | |||
*[[Thrombosis|Thrombosis]] | |||
*[[Myocardial infarction]] | |||
*[[Thrombosis|Thrombosis]] | |||
*[[Pulmonary embolism]] | |||
*[[Cardiogenic shock]] | |||
*Degeneration of the [[sinoatrial]] or [[atrioventricular]] nodes | |||
*[[Ischemic stroke]] | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" | | | style="padding: 5px 5px; background: #F5F5F5;" align="left" | | ||
* | * There is no electrical activity in the asystole | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" | | | style="padding: 5px 5px; background: #F5F5F5;" align="left" | | ||
[[Image:Lead II rhythm generated asystole.JPG|center|300px]] | |||
|- | |- | ||
! style="padding: 5px 5px; background: #DCDCDC;" align="left" | Pulseless electrical activity | ! style="padding: 5px 5px; background: #DCDCDC;" align="left" | Pulseless electrical activity<ref name="ECC_2005_7.2">"2005 American Heart Association Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care - Part 7.2: Management of Cardiac Arrest." ''Circulation'' 2005; '''112''': IV-58 - IV-66.</ref><ref>Foster B, Twelve Lead Electrocardiography, 2nd edition, 2007</ref> | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" | | | style="padding: 5px 5px; background: #F5F5F5;" align="left" | | ||
*Hypovolemia | *Hypovolemia | ||
Revision as of 20:04, 28 January 2020
Images

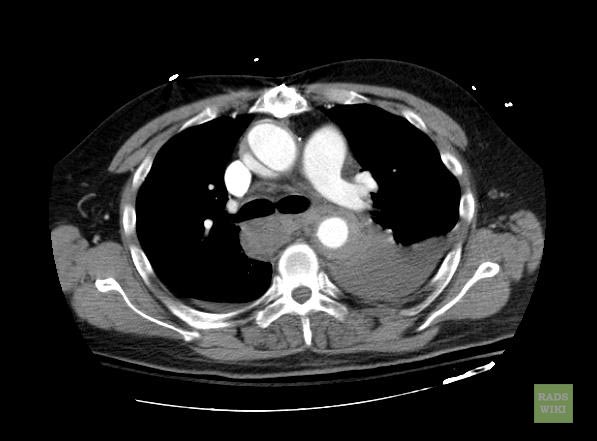
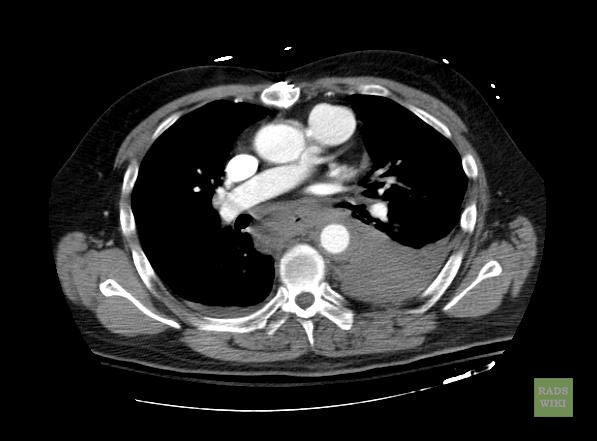
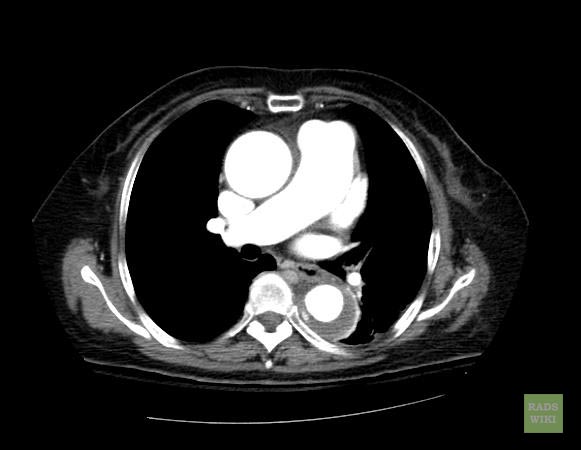

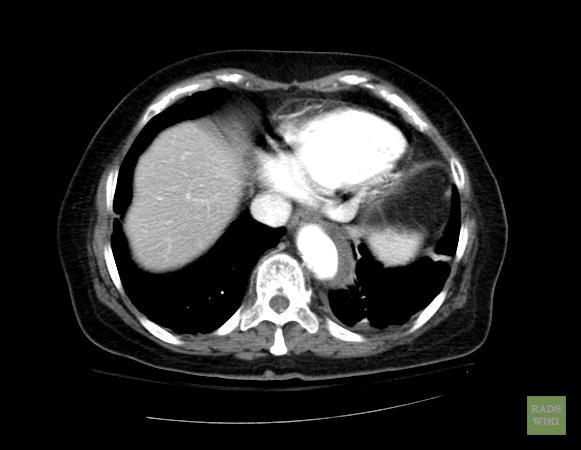
- Macura, Katarzyna J., Corl, Frank M., Fishman, Elliot K., Bluemke, David A. Pathogenesis in Acute Aortic Syndromes: Aortic Dissection, Intramural Hematoma, and Penetrating Atherosclerotic Aortic Ulcer. Am. J. Roentgenol. 2003 181: 309-316.
- Gomez-Jorge, Jackeline. E-medicine rads article
| Disease Name | Causes | ECG Characteristics | ECG view |
|---|---|---|---|
| Ventricular tachycardia[1][2][3][4] |
|
| |
| Ventricular fibrillation |
|
|
|
| Asystole[5][6] |
|
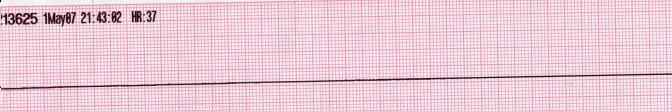 | |
| Pulseless electrical activity[7][8] |
|
|
 |
| Pulmonary embolism |
|
|
|
- ↑ Ajijola, Olujimi A.; Tung, Roderick; Shivkumar, Kalyanam (2014). "Ventricular tachycardia in ischemic heart disease substrates". Indian Heart Journal. 66: S24–S34. doi:10.1016/j.ihj.2013.12.039. ISSN 0019-4832.
- ↑ Meja Lopez, Eliany; Malhotra, Rohit (2019). "Ventricular Tachycardia in Structural Heart Disease". Journal of Innovations in Cardiac Rhythm Management. 10 (8): 3762–3773. doi:10.19102/icrm.2019.100801. ISSN 2156-3977.
- ↑ Coughtrie, Abigail L; Behr, Elijah R; Layton, Deborah; Marshall, Vanessa; Camm, A John; Shakir, Saad A W (2017). "Drugs and life-threatening ventricular arrhythmia risk: results from the DARE study cohort". BMJ Open. 7 (10): e016627. doi:10.1136/bmjopen-2017-016627. ISSN 2044-6055.
- ↑ El-Sherif, Nabil (2001). "Mechanism of Ventricular Arrhythmias in the Long QT Syndrome: On Hermeneutics". Journal of Cardiovascular Electrophysiology. 12 (8): 973–976. doi:10.1046/j.1540-8167.2001.00973.x. ISSN 1045-3873.
- ↑ ACLS: Principles and Practice. p. 71-87. Dallas: American Heart Association, 2003. ISBN 0-87493-341-2.
- ↑ ACLS for Experienced Providers. p. 3-5. Dallas: American Heart Association, 2003. ISBN 0-87493-424-9.
- ↑ "2005 American Heart Association Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care - Part 7.2: Management of Cardiac Arrest." Circulation 2005; 112: IV-58 - IV-66.
- ↑ Foster B, Twelve Lead Electrocardiography, 2nd edition, 2007
| Disease Name | Age of Onset | Gender Preponderance | Signs/Symptoms | Imaging Feature(s) | Macroscopic Feature(s) | Microscopic Feature(s) | Laboratory Findings(s) | Other Feature(s) | ECG view |
|---|---|---|---|---|---|---|---|---|---|