Sandbox:Roukoz: Difference between revisions
| Line 172: | Line 172: | ||
The presence of [finding(s)] on physical examination is highly suggestive of [disease name]. | The presence of [finding(s)] on physical examination is highly suggestive of [disease name]. | ||
*Signs and symptom s of protein S deficiency are those associated with deep venous thrombosis (DVT), thrombophlebitis, or pulmonary embolus. Some women may have fetal loss as their only manifestation of a thrombophilic disorder (eg, protein S deficiency). | |||
**With venous thrombosis of the lower limbs, lower limb swelling and discomfort are the usual symptoms. Occasionally, redness or discoloration also is present, with or without associated cellulitis. | |||
* | |||
===Laboratory Findings=== | ===Laboratory Findings=== | ||
Revision as of 16:53, 25 September 2018
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: Roukoz A. Karam, M.D.[2]
Overview
Protein S deficiency is an autosomal dominant thrombophilia, which leads to an increased risk of thromboembolic events. Protein S is a vitamin K-dependent glycoprotein and plays a role in anticoagulation. It is mainly a cofactor to the activated protein C (APC), which inactivates coagulation factors Va and VIIa and thereby controlling the coagulation cascade.
Historical Perspective
- Protein S was first discovered and purified in Seattle, Washington in 1979, and it was arbitrarily named protein S after the city it was discovered in.
- The function of this protein was still unknown; however, it was hypothesized that protein S plays a role in activating protein C.
- Protein S deficiency was first discovered in 1984 when two related individuals with recurrent thromboembolic events and normal coagulation tests were studied. At the time, protein C deficiency was usually associated with recurrent familial thrombosis. These individuals were found to have diminished anticoagulation activity with normal coagulation tests (including a normal protein C level), and when purified human protein S was added to their plasma, effective anticoagulation was restored. [1]
Classification
Protein S deficiency can be subdivided into three types depending on whether the abnormality affects total protein S level, free protein S level, and/or protein S function:[2]
- Type I: Reduced total protein S, free protein S, and protein S function
It is the classic form of hereditary protein S deficiency. Total protein S levels drop to approximately 50% of normal values while free protein S levels collapse to almost 15% of the normal. On a genetic level, type I deficiency usually results from missense or nonsense mutations. On few occasions, microinsertions, microdeletions, and splice site mutations have occurred with this type. [3]
- Type II: Normal total and free protein S, reduced protein S function
This form results from a qualitative defect and is very rare. The genetics behind this type isn't certain; however, some reports have linked it to missense mutations affecting the protein S's ability to bind to the activated protein C. [4] [5]
- Type III: Normal total protein S, reduced free protein S and protein S function
This is a quantitative defect.
| Type | Total Protein S | Free Protein S | Protein S Function |
|---|---|---|---|
| I | ↓ | ↓ | ↓ |
| II | ↔ | ↔ | ↓ |
| III | ↔ | ↓ | ↓ |
Pathophysiology
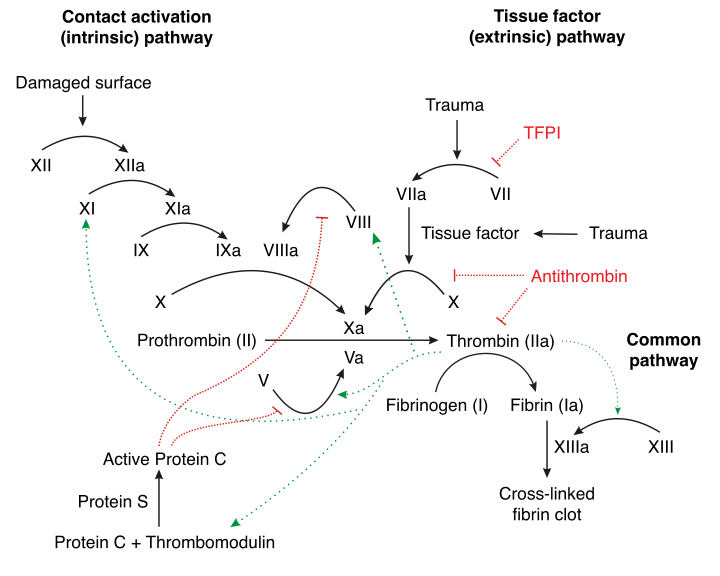 |
- Protein S is a natural anticoagulant that works with other proteins to regulate coagulation in the body.
- After it gets produced by the hepatocytes, endothelial cells, and megakaryocytes, protein S undergoes activation via vitamin K-dependent gamma-carboxylation. [7]
- The vitamin K-dependent gamma-carboxyalse enzyme acts by modifying the glutamic acid residues in protein S to gamma-carboxyglutamic acid residues.
- These gamma-carboxyglutamic acid residues are needed to ensure calcium-dependent binding to membrane surfaces.
- The now mature and activated protein S will circulate in the blood in two states:
- Free protein S
- This form constitutes 30 to 40 percent of the total protein S in the body.
- It is the only form that will take part in the coagulation cascade.[8]
- C4b-bound protein S
- There is a high affinity interaction between protein S and C4b-binding protein.
- C4b-binding protein is a complement regulator; hence, it is responsible for controlling the activity of protein S.
- Around 70 percent of circulating protein S is in the bound form. [9]
- Free protein S
- The activated free protein S acts as a cofactor to activated protein C, and with the help of phospholipids and Ca2+, it inactivates procoagulant factor Va and factor VIIIa thereby reducing thrombin formation.[7]
- Protein S deficiency is a hereditary disease that results from mutations in the PROS1 gene, located on chromosome 3.
- This disease usually occurs due to heterozygous gene mutations in the PROS1 gene; however, rare cases of homozygous protein S deficiencies have been reported.
- Although another gene, PROS2, has been isolated on the same chromosome 3, it does not seem to have any relevance and has since been classified as a pseudogene.[10][11]
Causes
- In addition to the common hereditary form of protein S deficiency, there are rare circumstances in which acquired causes can result in diminished protein S levels. These situations arise due to different mechanisms:[12]
Differentiating Protein S deficiency from Other Diseases
Protein S deficiency must be differentiated from other diseases that cause symptoms of DVT and pulmonary embolism such as:
- Factor V Leiden mutation
- Antithrombin III deficiency
- Protein C deficiency
- Prothrombin gene mutation
- Disseminated intravascular coagulation (DIC)
- Antiphospholipid antibody syndrome
For more information on differentiating protein S deficiency, click here.
Epidemiology and Demographics
- The prevalence of protein S deficiency in the general population is unknown.
- However, its prevalence in individuals with a history of venous thromboembolism is approximately 900 per 100,000 individuals worldwide. [19]
Age
- Patients of all age groups may be diagnosed with protein S deficiency.
- It is; however, more commonly observed among patients younger than 40 to 50 years old.
Gender
- There is no difference in the prevalence of the disease between men and women.
Race
- Protein S deficiency usually affects individuals of the Asian race.
- Caucasian individuals are less likely to develop protein S deficiency.
Risk Factors
- There are no established risk factors for protein S deficiency.
- Family history of thrombosis pose increased risk for a mutation.
Screening
- There is insufficient evidence to recommend routine screening for protein S deficiency in the general population.
- A simple positive family history incident of thrombosis is not enough to recommend screening in an asymptomatic low risk individual.[20]
- High risk patients with a positive family history (first degree relative with protein S deficiency or first degree relative with multiple venous thromboembolic events at an age younger than 50), warrant a screening preferably prior to initiation of the high risk event such as taking oral contraceptives or pregnancy.[21][22]
- The free protein S antigen assay is the best screening test.
Natural History, Complications, and Prognosis
If left untreated, [#]% of patients with [disease name] may progress to develop [manifestation 1], [manifestation 2], and [manifestation 3].
OR
Common complications of [disease name] include [complication 1], [complication 2], and [complication 3].
OR
Prognosis is generally excellent/good/poor, and the 1/5/10-year mortality/survival rate of patients with [disease name] is approximately [#]%.
Diagnosis
Diagnostic Study of Choice
- There is no established criteria for a definitive diagnosis of protein S deficiency.
- The diagnosis of protein S deficiency is the toughest out of all the hereditary thrombophilias due to protein S's interaction with other proteins, its complex genetic regulation, and its biologic variation.
- The diagnosis is made even more strenuous due to the the prevalence of acquired protein S deficiency causes (pregnancy, liver disease, DIC...).
- Three tests are used to assess protein S in plasma:[12][23]
- Free protein S antigen
- Determines free protein S level in plasma
- Most reliable of the three tests
- Evaluates the function of protein S indirectly
- ELISA technique
- Total protein S antigen
- Determines both free and bound protein S
- ELISA technique
- Protein S activity assay
- Assesses protein S's function as a cofactor for activated protein C
- Indirectly measured based on a coagulation assay and the time to clot
- Not very reliable due to inability to differentiate from factor V Leiden mutation (resistance to activated protein C)[24]
- Free protein S antigen
History and Symptoms
- The hallmark of protein S deficiency is venous thromboembolism.
- A positive history of a venous thromboembolic event prior to age 50, a strong family history of venous thromboembolic events, and/or a known protein S deficient family member is suggestive of a protein S deficiency.
- The most common sites of venous thromboembolism include deep vein thrombosis and pulmonary embolism.
- Less common sites of venous thromboembolism include cerebral, axillary, and mesenteric veins.
Physical Examination
Patients with [disease name] usually appear [general appearance]. Physical examination of patients with [disease name] is usually remarkable for [finding 1], [finding 2], and [finding 3].
OR
Common physical examination findings of [disease name] include [finding 1], [finding 2], and [finding 3].
OR
The presence of [finding(s)] on physical examination is diagnostic of [disease name].
OR
The presence of [finding(s)] on physical examination is highly suggestive of [disease name].
- Signs and symptom s of protein S deficiency are those associated with deep venous thrombosis (DVT), thrombophlebitis, or pulmonary embolus. Some women may have fetal loss as their only manifestation of a thrombophilic disorder (eg, protein S deficiency).
- With venous thrombosis of the lower limbs, lower limb swelling and discomfort are the usual symptoms. Occasionally, redness or discoloration also is present, with or without associated cellulitis.
Laboratory Findings
An elevated/reduced concentration of serum/blood/urinary/CSF/other [lab test] is diagnostic of [disease name].
OR
Laboratory findings consistent with the diagnosis of [disease name] include [abnormal test 1], [abnormal test 2], and [abnormal test 3].
OR
[Test] is usually normal among patients with [disease name].
OR
Some patients with [disease name] may have elevated/reduced concentration of [test], which is usually suggestive of [progression/complication].
OR
There are no diagnostic laboratory findings associated with [disease name].
Electrocardiogram
- There are no ECG findings associated with protein S deficiency.
X-ray
- There are no x-ray findings associated with protein S deficiency.
Echocardiography or Ultrasound
- There are no echocardiography/ultrasound findings associated with protein S deficiency.
CT scan
- There are no CT scan findings associated with protein S deficiency.
MRI
- There are no MRI findings associated with protein S deficiency.
Other Imaging Findings
- There are no other imaging findings associated with protein S deficiency.
Other Diagnostic Studies
- There are no other diagnostic studies associated with protein S deficiency.
Treatment
Medical Therapy
There is no treatment for [disease name]; the mainstay of therapy is supportive care.
OR
Supportive therapy for [disease name] includes [therapy 1], [therapy 2], and [therapy 3].
OR
The majority of cases of [disease name] are self-limited and require only supportive care.
OR
[Disease name] is a medical emergency and requires prompt treatment.
OR
The mainstay of treatment for [disease name] is [therapy].
OR The optimal therapy for [malignancy name] depends on the stage at diagnosis.
OR
[Therapy] is recommended among all patients who develop [disease name].
OR
Pharmacologic medical therapy is recommended among patients with [disease subclass 1], [disease subclass 2], and [disease subclass 3].
OR
Pharmacologic medical therapies for [disease name] include (either) [therapy 1], [therapy 2], and/or [therapy 3].
OR
Empiric therapy for [disease name] depends on [disease factor 1] and [disease factor 2].
OR
Patients with [disease subclass 1] are treated with [therapy 1], whereas patients with [disease subclass 2] are treated with [therapy 2].
Surgery
- Surgical intervention is not recommended for the management of protein S deficiency.
Primary Prevention
There are no established measures for the primary prevention of [disease name].
OR
There are no available vaccines against [disease name].
OR
Effective measures for the primary prevention of [disease name] include [measure1], [measure2], and [measure3].
OR
[Vaccine name] vaccine is recommended for [patient population] to prevent [disease name]. Other primary prevention strategies include [strategy 1], [strategy 2], and [strategy 3].
Secondary Prevention
There are no established measures for the secondary prevention of [disease name].
References
- ↑ Comp PC, Nixon RR, Cooper MR, Esmon CT (1984). "Familial protein S deficiency is associated with recurrent thrombosis". J Clin Invest. 74 (6): 2082–8. doi:10.1172/JCI111632. PMC 425398. PMID 6239877.
- ↑ Gandrille S, Borgel D, Sala N, Espinosa-Parrilla Y, Simmonds R, Rezende S; et al. (2000). "Protein S deficiency: a database of mutations--summary of the first update". Thromb Haemost. 84 (5): 918. PMID 11127877.
- ↑ Schwarz HP, Fischer M, Hopmeier P, Batard MA, Griffin JH (1984). "Plasma protein S deficiency in familial thrombotic disease". Blood. 64 (6): 1297–300. PMID 6238642.
- ↑ Simmonds RE, Ireland H, Kunz G, Lane DA (1996). "Identification of 19 protein S gene mutations in patients with phenotypic protein S deficiency and thrombosis. Protein S Study Group". Blood. 88 (11): 4195–204. PMID 8943854.
- ↑ Gandrille S, Borgel D, Eschwege-Gufflet V, Aillaud M, Dreyfus M, Matheron C; et al. (1995). "Identification of 15 different candidate causal point mutations and three polymorphisms in 19 patients with protein S deficiency using a scanning method for the analysis of the protein S active gene". Blood. 85 (1): 130–8. PMID 7803790.
- ↑ "Protein C - Wikipedia".
- ↑ 7.0 7.1 Esmon CT (1992). "Protein S and protein C Biochemistry, physiology, and clinical manifestation of deficiencies". Trends Cardiovasc Med. 2 (6): 214–9. doi:10.1016/1050-1738(92)90027-P. PMID 21239244.
- ↑ Rezende SM, Simmonds RE, Lane DA (2004). "Coagulation, inflammation, and apoptosis: different roles for protein S and the protein S-C4b binding protein complex". Blood. 103 (4): 1192–201. doi:10.1182/blood-2003-05-1551. PMID 12907438.
- ↑ Dahlbäck B (2011). "C4b-binding protein: a forgotten factor in thrombosis and hemostasis". Semin Thromb Hemost. 37 (4): 355–61. doi:10.1055/s-0031-1276584. PMID 21805441.
- ↑ Ploos van Amstel JK, van der Zanden AL, Bakker E, Reitsma PH, Bertina RM (1987). "Two genes homologous with human protein S cDNA are located on chromosome 3". Thromb Haemost. 58 (4): 982–7. PMID 2895503.
- ↑ Schmidel DK, Tatro AV, Phelps LG, Tomczak JA, Long GL (1990). "Organization of the human protein S genes". Biochemistry. 29 (34): 7845–52. PMID 2148110.
- ↑ 12.0 12.1 Marlar RA, Gausman JN (2011). "Protein S abnormalities: a diagnostic nightmare". Am J Hematol. 86 (5): 418–21. doi:10.1002/ajh.21992. PMID 21523802.
- ↑ Heeb MJ, Mosher D, Griffin JH (1989). "Activation and complexation of protein C and cleavage and decrease of protein S in plasma of patients with intravascular coagulation". Blood. 73 (2): 455–61. PMID 2521800.
- ↑ Comp PC, Doray D, Patton D, Esmon CT (1986). "An abnormal plasma distribution of protein S occurs in functional protein S deficiency". Blood. 67 (2): 504–8. PMID 2935211.
- ↑ Matsuzaka T, Tanaka H, Fukuda M, Aoki M, Tsuji Y, Kondoh H (1993). "Relationship between vitamin K dependent coagulation factors and anticoagulants (protein C and protein S) in neonatal vitamin K deficiency". Arch Dis Child. 68 (3 Spec No): 297–302. PMC 1590375. PMID 8466266.
- ↑ Comp PC, Thurnau GR, Welsh J, Esmon CT (1986). "Functional and immunologic protein S levels are decreased during pregnancy". Blood. 68 (4): 881–5. PMID 2944555.
- ↑ Gilabert J, Fernandez JA, España F, Aznar J, Estelles A (1988). "Physiological coagulation inhibitors (protein S, protein C and antithrombin III) in severe preeclamptic states and in users of oral contraceptives". Thromb Res. 49 (3): 319–29. PMID 2966452.
- ↑ Vigano-D'Angelo S, D'Angelo A, Kaufman CE, Sholer C, Esmon CT, Comp PC (1987). "Protein S deficiency occurs in the nephrotic syndrome". Ann Intern Med. 107 (1): 42–7. PMID 2954500.
- ↑ Pintao MC, Ribeiro DD, Bezemer ID, Garcia AA, de Visser MC, Doggen CJ; et al. (2013). "Protein S levels and the risk of venous thrombosis: results from the MEGA case-control study". Blood. 122 (18): 3210–9. doi:10.1182/blood-2013-04-499335. PMID 24014240.
- ↑ Wu O, Robertson L, Twaddle S, Lowe G, Clark P, Walker I; et al. (2005). "Screening for thrombophilia in high-risk situations: a meta-analysis and cost-effectiveness analysis". Br J Haematol. 131 (1): 80–90. doi:10.1111/j.1365-2141.2005.05715.x. PMID 16173967.
- ↑ Wu O, Robertson L, Langhorne P, Twaddle S, Lowe GD, Clark P; et al. (2005). "Oral contraceptives, hormone replacement therapy, thrombophilias and risk of venous thromboembolism: a systematic review. The Thrombosis: Risk and Economic Assessment of Thrombophilia Screening (TREATS) Study". Thromb Haemost. 94 (1): 17–25. doi:10.1160/TH04-11-0759. PMID 16113779.
- ↑ Dalen JE (2008). "Should patients with venous thromboembolism be screened for thrombophilia?". Am J Med. 121 (6): 458–63. doi:10.1016/j.amjmed.2007.10.042. PMID 18501222.
- ↑ Alshaikh NA, Rosing J, Thomassen MCLGD, Castoldi E, Simioni P, Hackeng TM (2017). "New functional assays to selectively quantify the activated protein C- and tissue factor pathway inhibitor-cofactor activities of protein S in plasma". J Thromb Haemost. 15 (5): 950–960. doi:10.1111/jth.13657. PMID 28211163.
- ↑ Faioni EM, Franchi F, Asti D, Sacchi E, Bernardi F, Mannucci PM (1993). "Resistance to activated protein C in nine thrombophilic families: interference in a protein S functional assay". Thromb Haemost. 70 (6): 1067–71. PMID 8165605.