Plummer-Vinson syndrome pathophysiology: Difference between revisions
Akshun Kalia (talk | contribs) No edit summary |
Akshun Kalia (talk | contribs) No edit summary |
||
| Line 1: | Line 1: | ||
__NOTOC__ | __NOTOC__ | ||
{{Plummer-Vinson syndrome}} | {{Plummer-Vinson syndrome}} | ||
{{CMG}} {{AE}} | {{CMG}}; {{AE}}{{Akshun}} | ||
==Overview== | ==Overview== | ||
Revision as of 14:17, 3 November 2017
|
Plummer-Vinson syndrome Microchapters |
|
Diagnosis |
|---|
|
Treatment |
|
Case Studies |
|
Plummer-Vinson syndrome pathophysiology On the Web |
|
American Roentgen Ray Society Images of Plummer-Vinson syndrome pathophysiology |
|
Risk calculators and risk factors for Plummer-Vinson syndrome pathophysiology |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: Akshun Kalia M.B.B.S.[2]
Overview
Plummer-Vinson syndrome is a rare condition characterized by iron-deficiency anemia, glossitis and dysphagia. The exact pathogenesis of Plummer-Vinson syndrome is not fully understood. It is postulated that Plummer-Vinson syndrome results from iron deficiency. Other possible factors include malnutrition, genetic predisposition and autoimmune disorders. In patients with iron deficiency, the iron-dependent oxidative enzymes are unable to function at optimum level and the dependent metabolic pathways (oxidative phosphorylation) are reduced. This promotes anaerobic metabolism with increased consumption of glucose and increased production of lactic acid and may lead to myasthenic changes in muscles. These myasthenic changes are often seen in muscles involved in swallowing and may lead to atrophy of the esophageal mucosa and formation of esophageal webs. Patients who do not exhibit obstructive lesions (web or stricture) may have dysphagia resulting from muscular in-coordination. Patients with iron deficiency have low levels of myoglobin which may affect the muscles of the tongue and lead to glossitis. In Plummer-Vinson syndrome, deficiency of iron can lead to epithelial atrophy and a decrease in the regenerative capacity of the mucosa. The decrease in rate of healing allows the chronic irritants to act progressively, predisposing the oral cavity and esophagus to malignant transformation (squamous cell carcinoma). Genes involved in the pathogenesis of iron deficiency anemia associated with Plummer-Vinson syndrome include mutation in TMPRSS6 gene. The TMPRSS6 gene encodes instructions for the protein hepcidin. Increased levels of hepcidin leads to decreased release of iron from ferritin and subsequently presents as iron deficiency anemia. On gross pathology, esophageal web and esophageal strictures are characteristic findings of Plummer-Vinson syndrome. On microscopic histopathological analysis, Plummer-Vinson syndrome presents with epithelial atrophy, chronic submucosal inflammation and epithelial atypia or dysplasia (in advanced cases)
Pathophysiology
Pathogenesis
- Plummer-Vinson syndrome is a rare condition characterized by iron-deficiency anemia, glossitis and dysphagia.
- The exact pathogenesis of Plummer-Vinson syndrome is not fully understood. It is postulated that Plummer-Vinson syndrome results from iron deficiency. Other possible factors include malnutrition, genetic predisposition and autoimmune disorders.[1][2][3][4]
- Iron plays a major role in the expression of citric acid cycle enzymes such as citrate synthase, isocitric dehydrogenase, and succinate dehydrogenase.
- Iron replete cells with normal citric acid cycle have an increased formation of reducing equivalents (NADH) thus leading to increased ATP formation via oxidative phosphorylation.
- In patients with iron deficiency, the iron-dependent oxidative enzymes are unable to function at optimum level and the dependent metabolic pathways (oxidative phosphorylation) are reduced.
- This promotes anaerobic metabolism with increased consumption of glucose and increased production of lactic acid and may lead to myasthenic changes in muscles.
- These myasthenic changes are often seen in muscles involved in swallowing and may lead to atrophy of the esophageal mucosa and formation of esophageal webs.
- The dysphagia in Plummer-Vinson syndrome results from esophageal (postcricoid) web or stricture. However, patients who do not exhibit obstructive lesions (web or stricture) may have dysphagia resulting from muscular in-coordination.
- Iron is also important in the synthesis of myoglobin which is responsible for meeting the energy demands of the muscle. Patients with iron deficiency have low levels of myoglobin which may affect the muscles of the tongue and lead to glossitis.
- In Plummer-Vinson syndrome, deficiency of iron can lead to epithelial atrophy and a decrease in the regenerative capacity of the mucosa. The decrease in rate of healing allows the chronic irritants to act progressively, predisposing the oral cavity and esophagus to malignant transformation (squamous cell carcinoma).
- Other factors involved in the pathogenesis of Plummer-Vinson syndrome include malnutrition, genetic predisposition and autoimmune disorders.[5][6][7][8][9][10]
- Plummer-Vinson syndrome is seen in certain genetically predisposed individuals (such as mutation in TMPRSS6 gene) and those with malnutrition.
- Patients of Plummer-Vinson syndrome have been associated with the presence of heterotopic gastric mucosa of the proximal esophagus (HGMPE).
- The HGMPE is also known as inlet patch or cervical inlet patch.
- HGMPE is a salmon colored patch and is located just distal to the upper esophageal sphincter.
- The HGMPE is associated with an increased laryngopharyngeal acid reflux and neoplastic transformation.
- Thus patients with HGMPE have been associated with an increased frequency of bleeding (iron deficiency anemia) and ulceration leading to formation of web like structures in the esophagus.
- Some researchers postulate that Plummer-Vinson syndrome may be due to an autoimmune condition. This can be attributed to the fact that Plummer-Vinson syndrome has been associated with other autoimmune conditions such as pernicious anemia, rheumatoid arthritis, autoimmune thyroiditis and celiac disease.[11][12][13]
Associated Conditions
- Celiac disease
- Pernicious anemia
- Rheumatoid arthritis
- Autoimmune thyroiditis
- Pharyngeal cancer
- Esophageal cancer
Genes
The gene(s) involved in the pathogenesis of Plummer-Vinson syndrome include:[14][15][16][17][16]
- Genes involved in the pathogenesis of iron deficiency anemia associated with Plummer-Vinson syndrome include mutation in TMPRSS6 gene.
- Mutation in TMPRSS6 gene results in Iron-refractory iron deficiency anemia (IRIDA)
- TMPRSS6 gene is located on long arm (q) of chromosome 21 at position 22q12.3.
- The TMPRSS6 gene encodes instructions for the protein hepcidin.
- At least 40 different types of mutations have been identified in the TMPRSS6 gene.
- Mutated TMPRSS6 gene leads to uninhibited production of hepcidin.
- Overproduction of hepcidin leads to internalization and degradation of ferroportin. Ferroportin is present in the basolateral membrane of duodenal cells and mediates the transfer of iron from duodenal cells to transferrin in blood.
- Increased levels of hepcidin leads to decreased release of iron from ferritin and subsequently presents as iron deficiency anemia.
Gross Pathology
- On gross pathology, esophageal web and esophageal strictures are characteristic findings of Plummer-Vinson syndrome.
Microscopic Pathology
On microscopic histopathological analysis, Plummer-Vinson syndrome presents with the following findings:
- Epithelial atrophy
- Chronic submucosal inflammation
- Epithelial atypia or dysplasia (in advanced cases)
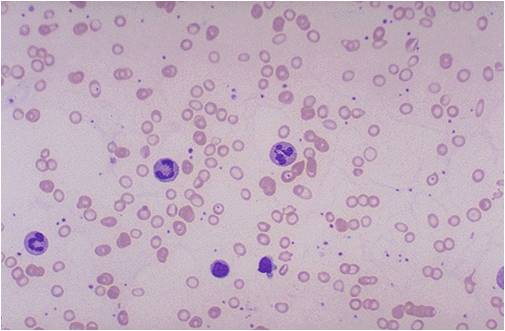
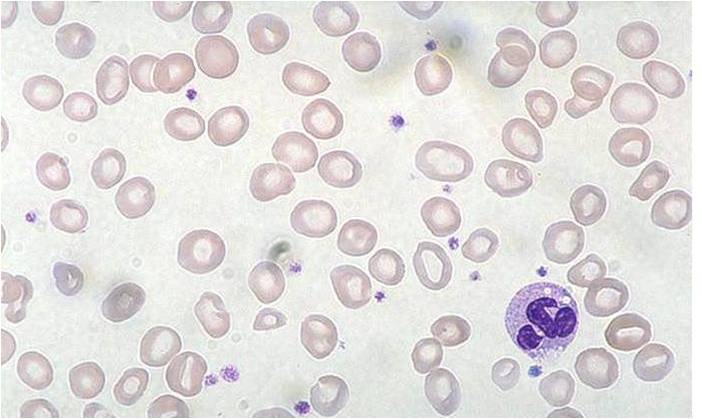
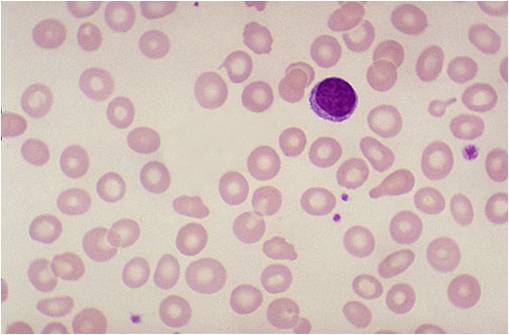
A peripheral blood smear in patients of Plummer-Vinson syndrome will present with:
- Hypochromia
- Microcytosis
- Increased platelet count
(Images shown below are courtesy of Melih Aktan MD, Istanbul Medical Faculty - Turkey)
-
Iron deficiency anemia
-
Iron deficiency anemia
-
Iron deficiency anemia
References
- ↑ Chisholm M (1974). "The association between webs, iron and post-cricoid carcinoma". Postgrad Med J. 50 (582): 215–9. PMC 2495558. PMID 4449772.
- ↑ Dantas RO, Villanova MG (1993). "Esophageal motility impairment in Plummer-Vinson syndrome. Correction by iron treatment". Dig. Dis. Sci. 38 (5): 968–71. PMID 8482199.
- ↑ Novacek G (2006). "Plummer-Vinson syndrome". Orphanet J Rare Dis. 1: 36. doi:10.1186/1750-1172-1-36. PMC 1586011. PMID 16978405.
- ↑ Ekberg O, Malmquist J, Lindgren S (1986). "Pharyngo-oesophageal webs in dysphageal patients. A radiologic and clinical investigation in 1134 patients". Rofo. 145 (1): 75–80. doi:10.1055/s-2008-1048889. PMID 3016824.
- ↑ Chong VH (2013). "Clinical significance of heterotopic gastric mucosal patch of the proximal esophagus". World J. Gastroenterol. 19 (3): 331–8. doi:10.3748/wjg.v19.i3.331. PMC 3554816. PMID 23372354.
- ↑ Buse PE, Zuckerman GR, Balfe DM (1993). "Cervical esophageal web associated with a patch of heterotopic gastric mucosa". Abdom Imaging. 18 (3): 227–8. PMID 8508079.
- ↑ Basseri B, Conklin JL, Mertens RB, Lo SK, Bellack GS, Shaye OA (2009). "Heterotopic gastric mucosa (inlet patch) in a patient with laryngopharyngeal reflux (LPR) and laryngeal carcinoma: a case report and review of literature". Dis. Esophagus. 22 (4): E1–5. doi:10.1111/j.1442-2050.2008.00915.x. PMID 19473208.
- ↑ Jerome-Zapadka KM, Clarke MR, Sekas G (1994). "Recurrent upper esophageal webs in association with heterotopic gastric mucosa: case report and literature review". Am. J. Gastroenterol. 89 (3): 421–4. PMID 8122657.
- ↑ Jabbari M, Goresky CA, Lough J, Yaffe C, Daly D, Côté C (1985). "The inlet patch: heterotopic gastric mucosa in the upper esophagus". Gastroenterology. 89 (2): 352–6. PMID 4007426.
- ↑ von Rahden BH, Stein HJ, Becker K, Liebermann-Meffert D, Siewert JR (2004). "Heterotopic gastric mucosa of the esophagus: literature-review and proposal of a clinicopathologic classification". Am. J. Gastroenterol. 99 (3): 543–51. doi:10.1111/j.1572-0241.2004.04082.x. PMID 15056100.
- ↑ Dickey W, McConnell B (1999). "Celiac disease presenting as the Paterson-Brown Kelly (Plummer-Vinson) syndrome". Am. J. Gastroenterol. 94 (2): 527–9. doi:10.1111/j.1572-0241.1999.889_r.x. PMID 10022662.
- ↑ Malhotra P, Kochhar R, Varma N, Kumari S, Jain S, Varma S (2000). "Paterson-Kelly syndrome and celiac disease--a rare combination". Indian J Gastroenterol. 19 (4): 191–2. PMID 11059192.
- ↑ ELWOOD PC, JACOBS A, PITMAN RG, ENTWISTLE CC (1964). "EPIDEMIOLOGY OF THE PATERSON-KELLY SYNDROME". Lancet. 2 (7362): 716–20. PMID 14193944.
- ↑ Pinto J, Nobre de Jesus G, Palma Anselmo M, Gonçalves L, Brás D, Madeira Lopes J, Meneses J, Victorino R, Faustino P (2017). "Iron Refractory Iron Deficiency Anemia in Dizygotic Twins Due to a Novel TMPRSS6 Gene Mutation in Addition to Polymorphisms Associated With High Susceptibility to Develop Ferropenic Anemia". J Investig Med High Impact Case Rep. 5 (2): 2324709617701776. doi:10.1177/2324709617701776. PMC 5405884. PMID 28491880.
- ↑ Yaish HM, Farrell CP, Christensen RD, MacQueen BC, Jackson LK, Trochez-Enciso J, Kaplan J, Ward DM, Salah WK, Phillips JD (2017). "Two novel mutations in TMPRSS6 associated with iron-refractory iron deficiency anemia in a mother and child". Blood Cells Mol. Dis. 65: 38–40. doi:10.1016/j.bcmd.2017.04.002. PMID 28460265.
- ↑ 16.0 16.1 Camaschella C, Silvestri L (2011). "Molecular mechanisms regulating hepcidin revealed by hepcidin disorders". ScientificWorldJournal. 11: 1357–66. doi:10.1100/tsw.2011.130. PMID 21789471.
- ↑ Franchini M, Montagnana M, Lippi G (2010). "Hepcidin and iron metabolism: from laboratory to clinical implications". Clin. Chim. Acta. 411 (21–22): 1565–9. doi:10.1016/j.cca.2010.07.003. PMID 20620132.