Zollinger-Ellison syndrome surgery: Difference between revisions
Jump to navigation
Jump to search
| Line 17: | Line 17: | ||
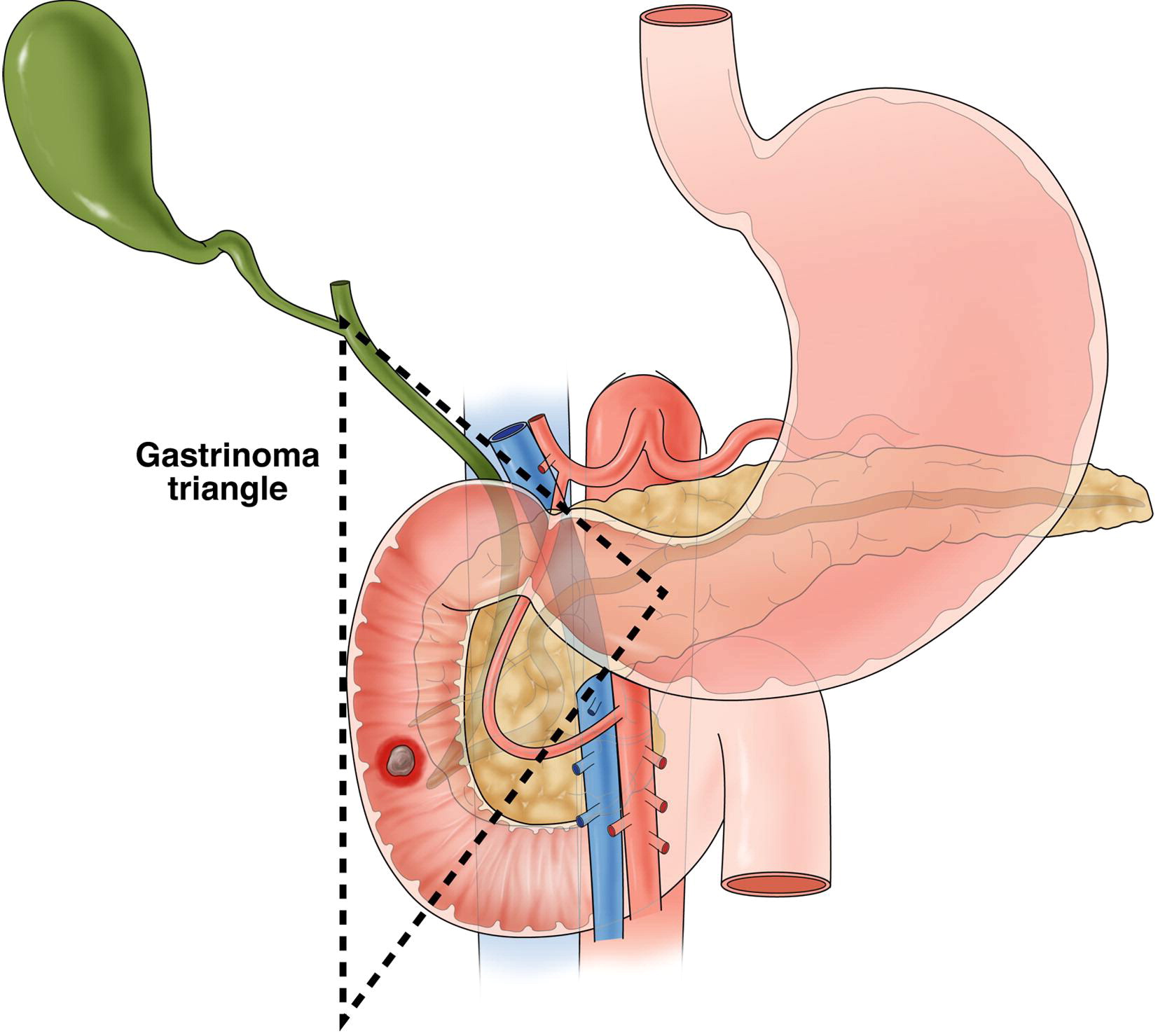
*Gastrinoma triangle borders are defined by confluence of the [[Cystic duct|cystic]] and [[common bile duct]] superiorly, the second and third portions of the [[duodenum]] inferiorly, and the neck and body of the [[pancreas]] medially, both dorsally and ventrally. <ref name="pmid24319020">{{cite journal |vauthors=Epelboym I, Mazeh H |title=Zollinger-Ellison syndrome: classical considerations and current controversies |journal=Oncologist |volume=19 |issue=1 |pages=44–50 |year=2014 |pmid=24319020 |pmc=3903066 |doi=10.1634/theoncologist.2013-0369 |url=}}</ref> | *Gastrinoma triangle borders are defined by confluence of the [[Cystic duct|cystic]] and [[common bile duct]] superiorly, the second and third portions of the [[duodenum]] inferiorly, and the neck and body of the [[pancreas]] medially, both dorsally and ventrally. <ref name="pmid24319020">{{cite journal |vauthors=Epelboym I, Mazeh H |title=Zollinger-Ellison syndrome: classical considerations and current controversies |journal=Oncologist |volume=19 |issue=1 |pages=44–50 |year=2014 |pmid=24319020 |pmc=3903066 |doi=10.1634/theoncologist.2013-0369 |url=}}</ref> | ||
[[Image:ZES_- | [[Image:ZES_-_GASTRINOMA_TRIANGLE_2.jpg|center|400px]]. | ||
==References== | ==References== | ||
Revision as of 18:59, 3 August 2017
|
Zollinger-Ellison syndrome Microchapters |
|
Differentiating Zollinger-Ellison syndrome from other Diseases |
|---|
|
Diagnosis |
|
Treatment |
|
Case Studies |
|
Zollinger-Ellison syndrome surgery On the Web |
|
American Roentgen Ray Society Images of Zollinger-Ellison syndrome surgery |
|
Risk calculators and risk factors for Zollinger-Ellison syndrome surgery |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: Aravind Reddy Kothagadi M.B.B.S[2]; Mohamad Alkateb, MBBCh [3]
Overview
The feasibility of surgery depends on the stage of gastrinoma causing Zollinger-Ellison syndrome at the time of diagnosis. However, all patients diagnosed with Zollinger-Ellison syndrome with no metastasis should be offered surgical exploration and resection.
Surgery
- With the advent of inexpensive, easy to administer, and well-tolerated pharmacologic options, acid-reducing surgical procedures largely fell by the wayside, instead replaced by the highly effective medical therapy. [1]
- The role of surgical management of ZES has instead shifted to eradication of primary tumor and control/prevention of metastatic spread. [1]
- Surgical approach to gastrinoma differs in sporadic ZES and ZES associated with MEN-1. As already mentioned, even although many gastrinomas are well-differentiated, over half do carry malignant potential and mortality results from metastatic disease. [2]
- Even though for the most part gastrinomas are slow-growing tumors, and their metastatic propensity is low if the lesion is less than 2 cm in size, presence of metastatic disease dramatically worsens prognosis and decreases survival. Because of this, early surgical exploration and excision of primary lesions is done in patients with ZES to prevent distant spread. Unfortunately, complete surgical resection is possible in less than half of patients with sporadic ZES and not at all in patients who also have MEN-1. [3]
- The vast majority of gastrinomas are present within the “gastrinoma triangle,” which is composed of the porta hepatis, duodenal sweep, and pancreatic head. As surgery remains the treatment of choice, localization of the primary lesion is often challenging but essential. [4]
- The feasibility of surgery depends on the stage of gastrinoma causing Zollinger-Ellison syndrome at the time of diagnosis. However, all patients diagnosed with Zollinger-Ellison syndrome with no metastasis should be offered surgical exploration and resection.[5]
Gastrinoma Triangle
- Gastrinoma triangle borders are defined by confluence of the cystic and common bile duct superiorly, the second and third portions of the duodenum inferiorly, and the neck and body of the pancreas medially, both dorsally and ventrally. [6]
.
References
- ↑ 1.0 1.1 Norton JA, Fraker DL, Alexander HR, Gibril F, Liewehr DJ, Venzon DJ; et al. (2006). "Surgery increases survival in patients with gastrinoma". Ann Surg. 244 (3): 410–9. doi:10.1097/01.sla.0000234802.44320.a5. PMC 1856542. PMID 16926567.
- ↑ Norton JA, Jensen RT (2003). "Current surgical management of Zollinger-Ellison syndrome (ZES) in patients without multiple endocrine neoplasia-type 1 (MEN1)". Surg Oncol. 12 (2): 145–51. PMID 12946485.
- ↑ Norton JA (2005). "Surgical treatment and prognosis of gastrinoma". Best Pract Res Clin Gastroenterol. 19 (5): 799–805. doi:10.1016/j.bpg.2005.05.003. PMID 16253901.
- ↑ Yang RH, Chu YK (2015). "Zollinger-Ellison syndrome: Revelation of the gastrinoma triangle". Radiol Case Rep. 10 (1): 827. doi:10.2484/rcr.v10i1.827. PMC 4921170. PMID 27408649.
- ↑ Norton JA, Fraker DL, Alexander HR, Venzon DJ, Doppman JL, Serrano J; et al. (1999). "Surgery to cure the Zollinger-Ellison syndrome". N Engl J Med. 341 (9): 635–44. doi:10.1056/NEJM199908263410902. PMID 10460814.
- ↑ Epelboym I, Mazeh H (2014). "Zollinger-Ellison syndrome: classical considerations and current controversies". Oncologist. 19 (1): 44–50. doi:10.1634/theoncologist.2013-0369. PMC 3903066. PMID 24319020.