WBR0189: Difference between revisions
Ochuko Ajari (talk | contribs) (Created page with "{{WBRQuestion |QuestionAuthor=Ogheneochuko Ajari MB.BS., MS |ExamType=USMLE Step 1 |MainCategory=Microbiology |SubCategory=Infectious Disease |MainCategory=Microbiology |SubCa...") |
m (refreshing WBR questions) |
||
| (13 intermediate revisions by 3 users not shown) | |||
| Line 1: | Line 1: | ||
{{WBRQuestion | {{WBRQuestion | ||
|QuestionAuthor= | |QuestionAuthor= {{Ochuko}} (Reviewed by Will Gibson and {{YD}}) | ||
|ExamType=USMLE Step 1 | |ExamType=USMLE Step 1 | ||
|MainCategory=Microbiology | |MainCategory=Microbiology | ||
| Line 8: | Line 8: | ||
|MainCategory=Microbiology | |MainCategory=Microbiology | ||
|SubCategory=Infectious Disease | |SubCategory=Infectious Disease | ||
|MainCategory=Microbiology | |||
|MainCategory=Microbiology | |MainCategory=Microbiology | ||
|MainCategory=Microbiology | |MainCategory=Microbiology | ||
| Line 20: | Line 21: | ||
|MainCategory=Microbiology | |MainCategory=Microbiology | ||
|SubCategory=Infectious Disease | |SubCategory=Infectious Disease | ||
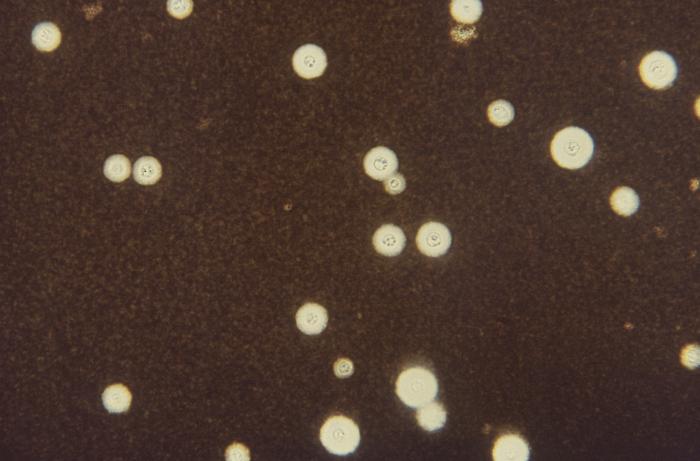
|Prompt=A | |Prompt=A 55-year-old HIV-positive woman is brought to the emergency department (ED) with complaints of headache, fever, and altered mental status for the past 6 days. Her daughter reports that the patient has been non-complaint with her antiretroviral therapy and has had no follow-up for several months. The patient's temperature is 39.2 °C (102.5 °F), blood pressure is 145/92 mmHg, heart rate is 104/min, and respiratory rate is 26/min. On physical examination, Kernig and Brudzinski signs are negative and no focal neurological deficits are noted. Work-up in the ED demonstrates a CD4 count of 40 cells/mm<sup>3</sup>. CSF examination with dye reveals the findings in the image below. Which of the following best describes the organism responsible for this patient's symptoms?<br> | ||
[[Image:WBR0189.jpg | 500px]] | |||
|Explanation=[[Cryptococcal meningitis]] is an opportunistic infection caused by ''[[Cryptococcus neoformans]]'' that is common among patients with AIDS and other causes of immunosuppression. While immunocompetent individuals may remain asymptomatic or develop granulomata to contain the infection, immunocompromised patients with CD4 count < 50 cells/mm<sup>3</sup> are at high risk of systemic infection with ''Cryptococcus neoformans'' and development of pulmonary disease with severe extrapulmonary complications, such as cryptococcal meningitis. The yeast are often found in the soil and in pigeon droppings; they are thought to be transmitted to the human host by inhalation of small yeast cells. ''C. neoformans'' utilizes several virulence factors to survive and evade the immune system. First, it is able to grow at 37 °C. Second, its capsule has antiphagocytic properties. Third, it expresses laccase to form melanin that interferes with oxidative killing of phagocytes. Finally, it may replicate intracellularly within the macrophages. Since ''C. neoformans'' is inhaled, the lungs are usually infected first, and patients often have mild or no pulmonary symptoms. Involvement of the CNS is a common complication, whereby patients develop subacute or chronic meningitis (or meningoencephalitis). Characteristically, patients with cryptococcal meningitis have symptoms of meningoencephalitis for several days but commonly have few or no classical signs of meningitis on physical examination (papilledema, palsies, focal neurological deficit, Kernig and Brudzinski signs). Nonetheless, the development of these signs is still widely reported. Prior to lumbar puncture, a CT-scan is necessary first for its possible contribution in the diagnosis of cryptococcal meningitis (gelatinous cryptococcal pseudocysts that give a soap bubble appearance may be observed); and more importantly, to rule out any findings that may suggest increased [[intracranial pressure]] (ICP). | |||
|AnswerE= | There are several methods to diagnose cryptococcal meningitis. The first is to examine the CSF microscopically for encapsulated yeast. This assay can be supplemented with an India Ink stain, as the capsule of the yeast will stain positively with the dye. The second method of rapid diagnosis is with a latex agglutination test. In this test, latex beads are coated with antibodies against the cryptococcal capsular antigen. If the antigen is present in a CSF sample that is mixed with the beads, the beads will agglutinate. The organism can be cultured in Sabourad's agar. However, treatment is often initiated based on clinical suspicion before culture results are conclusive. Patients with confirmed cryptococcal meningitis should be administered antifungal regimen with high-dose ''Amphotericin B'' plus flucytosine for the acute disease followed by oral fluconazole for maintenance therapy. | ||
|AnswerEExp= | |AnswerA=Dimorphic, encapsulated yeast | ||
|AnswerAExp=''Cryptococcus neoformans'' is a monomorphic encapsulated fungal pathogen. | |||
|AnswerB=Monomorphic, encapsulated yeast | |||
|AnswerBExp=Monomorphic encapsulated yeast describes ''Cryptococcus neoformans'', which is the causative agent in this vignette. | |||
|AnswerC=Yeast with broad-based budding | |||
|AnswerCExp=Broad-based budding yeast describes ''[[Blastomyces dermatitidis]]''. ''B. dermatitidis'' is the rarest of the systemic mycoses and causes chronic inflammatory lung disease. It is endemic to the Mississippi river valley. However, it is not a common cause of meningitis among HIV-positive patients. | |||
|AnswerD=Septate hyphae with branching at 45° angles | |||
|AnswerDExp=''[[Aspergillus fumigatus]]'' consists of branching septate hyphae. ''A. fumigatus'' is not a common cause of meningitis among HIV-positive patients. | |||
|AnswerE=Spaghetti and meatballs appearance on KOH stain | |||
|AnswerEExp=Spaghetti and meatballs on KOH stain describes ''[[Malassezia furfur]]'', the causative agent of [[tinea versicolor]]. | |||
|EducationalObjectives=''Cryptococcus neoformans'' is a monomorphic, encapsulated yeast that commonly causes subacute/chronic meningitis among HIV patients. | |||
|References=Perfect JR, Dismukes WE, Dromer F, et al. Clinical practice guidelines for the management of cryptococcal disease: 2010 update by the infectious diseases society of america. Clin Infect Dis. 2010;50(3):291-322.<br> Speed B, Dunt D. Clinical and host differences between infections with the two varieties of Cryptococcus neoformans. Clin Infect Dis. 1995;21(1):28-34.<br> | |||
Bicanic T, Harrison TS. Cryptococcal meningitis. Br Med Bull. 2004;72(1):99-118.<br> | |||
First Aid 2014 page 148 | |||
|RightAnswer=B | |RightAnswer=B | ||
|WBRKeyword=Cryptococcus, Cryptococcus neoformans, HIV, Opportunistic infection, Fungus, Yeast, Cryptococcal meningitis, Fever, Meningitis, Encephalitis | |||
|Approved=Yes | |Approved=Yes | ||
}} | }} | ||
Latest revision as of 23:41, 27 October 2020
| Author | [[PageAuthor::Ogheneochuko Ajari, MB.BS, MS [1] (Reviewed by Will Gibson and Yazan Daaboul, M.D.)]] |
|---|---|
| Exam Type | ExamType::USMLE Step 1 |
| Main Category | MainCategory::Microbiology |
| Sub Category | SubCategory::Infectious Disease |
| Prompt | [[Prompt::A 55-year-old HIV-positive woman is brought to the emergency department (ED) with complaints of headache, fever, and altered mental status for the past 6 days. Her daughter reports that the patient has been non-complaint with her antiretroviral therapy and has had no follow-up for several months. The patient's temperature is 39.2 °C (102.5 °F), blood pressure is 145/92 mmHg, heart rate is 104/min, and respiratory rate is 26/min. On physical examination, Kernig and Brudzinski signs are negative and no focal neurological deficits are noted. Work-up in the ED demonstrates a CD4 count of 40 cells/mm3. CSF examination with dye reveals the findings in the image below. Which of the following best describes the organism responsible for this patient's symptoms? |
| Answer A | AnswerA::Dimorphic, encapsulated yeast |
| Answer A Explanation | AnswerAExp::''Cryptococcus neoformans'' is a monomorphic encapsulated fungal pathogen. |
| Answer B | AnswerB::Monomorphic, encapsulated yeast |
| Answer B Explanation | AnswerBExp::Monomorphic encapsulated yeast describes ''Cryptococcus neoformans'', which is the causative agent in this vignette. |
| Answer C | AnswerC::Yeast with broad-based budding |
| Answer C Explanation | [[AnswerCExp::Broad-based budding yeast describes Blastomyces dermatitidis. B. dermatitidis is the rarest of the systemic mycoses and causes chronic inflammatory lung disease. It is endemic to the Mississippi river valley. However, it is not a common cause of meningitis among HIV-positive patients.]] |
| Answer D | AnswerD::Septate hyphae with branching at 45° angles |
| Answer D Explanation | [[AnswerDExp::Aspergillus fumigatus consists of branching septate hyphae. A. fumigatus is not a common cause of meningitis among HIV-positive patients.]] |
| Answer E | AnswerE::Spaghetti and meatballs appearance on KOH stain |
| Answer E Explanation | [[AnswerEExp::Spaghetti and meatballs on KOH stain describes Malassezia furfur, the causative agent of tinea versicolor.]] |
| Right Answer | RightAnswer::B |
| Explanation | [[Explanation::Cryptococcal meningitis is an opportunistic infection caused by Cryptococcus neoformans that is common among patients with AIDS and other causes of immunosuppression. While immunocompetent individuals may remain asymptomatic or develop granulomata to contain the infection, immunocompromised patients with CD4 count < 50 cells/mm3 are at high risk of systemic infection with Cryptococcus neoformans and development of pulmonary disease with severe extrapulmonary complications, such as cryptococcal meningitis. The yeast are often found in the soil and in pigeon droppings; they are thought to be transmitted to the human host by inhalation of small yeast cells. C. neoformans utilizes several virulence factors to survive and evade the immune system. First, it is able to grow at 37 °C. Second, its capsule has antiphagocytic properties. Third, it expresses laccase to form melanin that interferes with oxidative killing of phagocytes. Finally, it may replicate intracellularly within the macrophages. Since C. neoformans is inhaled, the lungs are usually infected first, and patients often have mild or no pulmonary symptoms. Involvement of the CNS is a common complication, whereby patients develop subacute or chronic meningitis (or meningoencephalitis). Characteristically, patients with cryptococcal meningitis have symptoms of meningoencephalitis for several days but commonly have few or no classical signs of meningitis on physical examination (papilledema, palsies, focal neurological deficit, Kernig and Brudzinski signs). Nonetheless, the development of these signs is still widely reported. Prior to lumbar puncture, a CT-scan is necessary first for its possible contribution in the diagnosis of cryptococcal meningitis (gelatinous cryptococcal pseudocysts that give a soap bubble appearance may be observed); and more importantly, to rule out any findings that may suggest increased intracranial pressure (ICP).
There are several methods to diagnose cryptococcal meningitis. The first is to examine the CSF microscopically for encapsulated yeast. This assay can be supplemented with an India Ink stain, as the capsule of the yeast will stain positively with the dye. The second method of rapid diagnosis is with a latex agglutination test. In this test, latex beads are coated with antibodies against the cryptococcal capsular antigen. If the antigen is present in a CSF sample that is mixed with the beads, the beads will agglutinate. The organism can be cultured in Sabourad's agar. However, treatment is often initiated based on clinical suspicion before culture results are conclusive. Patients with confirmed cryptococcal meningitis should be administered antifungal regimen with high-dose Amphotericin B plus flucytosine for the acute disease followed by oral fluconazole for maintenance therapy. |
| Approved | Approved::Yes |
| Keyword | WBRKeyword::Cryptococcus, WBRKeyword::Cryptococcus neoformans, WBRKeyword::HIV, WBRKeyword::Opportunistic infection, WBRKeyword::Fungus, WBRKeyword::Yeast, WBRKeyword::Cryptococcal meningitis, WBRKeyword::Fever, WBRKeyword::Meningitis, WBRKeyword::Encephalitis |
| Linked Question | Linked:: |
| Order in Linked Questions | LinkedOrder:: |