Dermatofibroma history and symptoms: Difference between revisions
Jump to navigation
Jump to search
Homa Najafi (talk | contribs) No edit summary |
m (Bot: Removing from Primary care) |
||
| (7 intermediate revisions by 3 users not shown) | |||
| Line 5: | Line 5: | ||
==Overview== | ==Overview== | ||
The majority of [[patients]] with dermatofibroma are [[asymptomatic]]. Dermatofibroma mostly develops as a single slow growing [[lesion]] on an extremity. Traumatized [[lesion]] may cause [[pain]], [[bleeding]], i[[Itching|tching]], erosive changes,and [[ulceration]]. Multiple dermatofibromas is a [[rare]] variant of [[disease]] which mostly seen in [[patients]] with underlying [[systemic]] [[disorders]]. | |||
==History and Symptoms== | ==History and Symptoms== | ||
*The majority of patients with [ | *The majority of [[patients]] with dermatofibroma are [[asymptomatic]]. <ref name="LeeLee2015">{{cite journal|last1=Lee|first1=MiWoo|last2=Lee|first2=WooJin|last3=Jung|first3=JoonMin|last4=Won|first4=ChongHyun|last5=Chang|first5=SungEun|last6=Choi|first6=JeeHo|last7=Moon|first7=KeeChan|title=Clinical and histological patterns of dermatofibroma without gross skin surface change: A comparative study with conventional dermatofibroma|journal=Indian Journal of Dermatology, Venereology, and Leprology|volume=81|issue=3|year=2015|pages=263|issn=0378-6323|doi=10.4103/0378-6323.154795}}</ref> | ||
*Dermatofibroma mostly develops as a single slow growing [[lesion]] on an extremity. | |||
* | *Traumatized [[lesion]] may cause:<ref name="NaversenTrask1993">{{cite journal|last1=Naversen|first1=Douglas N.|last2=Trask|first2=David M.|last3=Watson|first3=Frank H.|last4=Burket|first4=John M.|title=Painful tumors of the skin: “LEND AN EGG”|journal=Journal of the American Academy of Dermatology|volume=28|issue=2|year=1993|pages=298–300|issn=01909622|doi=10.1016/0190-9622(93)70039-V}}</ref> | ||
* | **[[Pain]] | ||
Dermatofibromas | **[[Bleeding]] | ||
**[[Itching]] | |||
**Erosive changes | |||
**[[Ulceration]] | |||
*Multiple dermatofibromas is a [[rare]] variant of [[disease]] which mostly seen in [[patients]] with underlying [[systemic]] [[disorders]]. <ref name="BhattacharjeeUmar2005">{{cite journal|last1=Bhattacharjee|first1=Pradip|last2=Umar|first2=Saleem|last3=Fatteh|first3=Shokat|title=Multiple Eruptive Dermatofibromas Occurring in a Patient with Myelodysplastic Syndrome|journal=Acta Dermato-Venereologica|volume=-1|issue=1|year=2005|pages=1–1|issn=0001-5555|doi=10.1080/00015550410024517}}</ref><ref>{{Cite journal | |||
| author = [[I. Lu]], [[P. R. Cohen]] & [[M. E. Grossman]] | |||
| title = Multiple dermatofibromas in a woman with HIV infection and systemic lupus erythematosus | |||
| journal = [[Journal of the American Academy of Dermatology]] | |||
| volume = 32 | |||
| issue = 5 Pt 2 | |||
| pages = 901–903 | |||
| year = 1995 | |||
| month = | |||
| doi = 10.1016/0190-9622(95)91558-3 | |||
| pmid = 7722054 | |||
|url=|first=|date=|via=}}</ref><ref>{{Cite journal | |||
| author = [[P. R. Cohen]] | |||
=== | | title = Multiple dermatofibromas in patients with autoimmune disorders receiving immunosuppressive therapy | ||
| journal = [[International journal of dermatology]] | |||
| volume = 30 | |||
| issue = 4 | |||
| pages = 266–270 | |||
| year = 1991 | |||
=== | | month = | ||
| pmid = 2050454 | |||
|url=|first=|date=|via=}}</ref><ref>{{Cite journal | |||
| author = [[Mayuri Tanaka]], [[Toshihiko Hoashi]], [[Naotaka Serizawa]], [[Kyochika Okabe]], [[Susumu Ichiyama]], [[Rie Shinohara]], [[Yoko Funasaka]] & [[Hidehisa Saeki]] | |||
| title = Multiple unilaterally localized dermatofibromas in a patient with Down syndrome | |||
| journal = [[The Journal of dermatology]] | |||
| volume = 44 | |||
| issue = 9 | |||
| pages = 1074–1076 | |||
| year = 2017 | |||
| month = | |||
| doi = 10.1111/1346-8138.13625 | |||
| pmid = 27665731 | |||
|url=|first=|date=|via=}}</ref><ref>{{Cite journal | |||
| author = [[J. Stainforth]] & [[M. J. Goodfield]] | |||
| title = Multiple dermatofibromata developing during pregnancy | |||
| journal = [[Clinical and experimental dermatology]] | |||
| volume = 19 | |||
| issue = 1 | |||
| pages = 59–60 | |||
| year = 1994 | |||
| month = | |||
| pmid = 8313640 | |||
|url=|first=|date=|via=}}</ref><ref>{{Cite journal | |||
| author = [[Yuichiro Tsunemi]], [[Hironobu Ihn]], [[Naoko Hattori]], [[Hidehisa Saeki]] & [[Kunihiko Tamaki]] | |||
| title = Multiple eruptive dermatofibromas with CD34+ cells in a patient with hypertriglyceridemia | |||
| journal = [[Dermatology (Basel, Switzerland)]] | |||
| volume = 207 | |||
| issue = 3 | |||
| pages = 319–321 | |||
| year = 2003 | |||
| month = | |||
| doi = 10.1159/000073098 | |||
| pmid = 14571078 | |||
}}</ref><ref>{{Cite journal | |||
| author = [[H. B. Bargman]] & [[I. Fefferman]] | |||
| title = Multiple dermatofibromas in a patient with myasthenia gravis treated with prednisone and cyclophosphamide | |||
| journal = [[Journal of the American Academy of Dermatology]] | |||
| volume = 14 | |||
| issue = 2 Pt 2 | |||
| pages = 351–352 | |||
| year = 1986 | |||
| month = | |||
| doi = 10.1016/s0190-9622(86)70041-8 | |||
| pmid = 3950136 | |||
|url=|first=|date=|via=}}</ref><ref>{{Cite journal | |||
| author = [[S. E. Chang]], [[J. H. Choi]], [[K. J. Sung]], [[K. C. Moon]] & [[J. K. Koh]] | |||
| title = Multiple eruptive dermatofibromas occurring in a patient with acute myeloid leukaemia | |||
| journal = [[The British journal of dermatology]] | |||
| volume = 142 | |||
| issue = 5 | |||
| pages = 1062–1063 | |||
| year = 2000 | |||
| month = | |||
| doi = 10.1046/j.1365-2133.2000.03508.x | |||
| pmid = 10809884 | |||
|url=|first=|date=|via=}}</ref> | |||
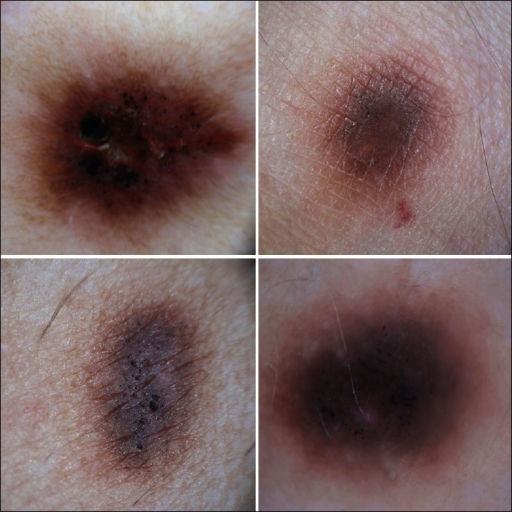
[[File:Dermatofibroma.jpg|200px|thumb|Contributed by creative commons|center]] | |||
[[File:Dermoscopy of dermatofibroma.png|350px|thumb|https://openi.nlm.nih.gov/detailedresult?img=PMC3667312_IJD-58-243a-g003&query=&req=4|center]] | |||
[[File:Multiple dermatofibromas.png|200px|thumb|https://openi.nlm.nih.gov/detailedresult?img=PMC3875973_abd-88-06-s1-0063-g05&query=&req=4|center]] | |||
==References== | ==References== | ||
{{Reflist|2}} | {{Reflist|2}} | ||
| Line 60: | Line 101: | ||
[[Category:Medicine]] | [[Category:Medicine]] | ||
[[Category:Oncology]] | [[Category:Oncology]] | ||
[[Category:Up-To-Date | [[Category:Up-To-Date]] | ||
[[Category:Dermatology]] | [[Category:Dermatology]] | ||
Latest revision as of 21:17, 29 July 2020
|
Dermatofibroma Microchapters |
|
Diagnosis |
|---|
|
Treatment |
|
Case Studies |
|
Dermatofibroma history and symptoms On the Web |
|
American Roentgen Ray Society Images of Dermatofibroma history and symptoms |
|
Risk calculators and risk factors for Dermatofibroma history and symptoms |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1];Associate Editor(s)-in-Chief: Homa Najafi, M.D.[2]
Overview
The majority of patients with dermatofibroma are asymptomatic. Dermatofibroma mostly develops as a single slow growing lesion on an extremity. Traumatized lesion may cause pain, bleeding, itching, erosive changes,and ulceration. Multiple dermatofibromas is a rare variant of disease which mostly seen in patients with underlying systemic disorders.
History and Symptoms
- The majority of patients with dermatofibroma are asymptomatic. [1]
- Dermatofibroma mostly develops as a single slow growing lesion on an extremity.
- Traumatized lesion may cause:[2]
- Pain
- Bleeding
- Itching
- Erosive changes
- Ulceration
- Multiple dermatofibromas is a rare variant of disease which mostly seen in patients with underlying systemic disorders. [3][4][5][6][7][8][9][10]


References
- ↑ Lee, MiWoo; Lee, WooJin; Jung, JoonMin; Won, ChongHyun; Chang, SungEun; Choi, JeeHo; Moon, KeeChan (2015). "Clinical and histological patterns of dermatofibroma without gross skin surface change: A comparative study with conventional dermatofibroma". Indian Journal of Dermatology, Venereology, and Leprology. 81 (3): 263. doi:10.4103/0378-6323.154795. ISSN 0378-6323.
- ↑ Bhattacharjee, Pradip; Umar, Saleem; Fatteh, Shokat (2005). "Multiple Eruptive Dermatofibromas Occurring in a Patient with Myelodysplastic Syndrome". Acta Dermato-Venereologica. -1 (1): 1–1. doi:10.1080/00015550410024517. ISSN 0001-5555.
- ↑ I. Lu, P. R. Cohen & M. E. Grossman (1995). "Multiple dermatofibromas in a woman with HIV infection and systemic lupus erythematosus". Journal of the American Academy of Dermatology. 32 (5 Pt 2): 901–903. doi:10.1016/0190-9622(95)91558-3. PMID 7722054.
- ↑ P. R. Cohen (1991). "Multiple dermatofibromas in patients with autoimmune disorders receiving immunosuppressive therapy". International journal of dermatology. 30 (4): 266–270. PMID 2050454.
- ↑ Mayuri Tanaka, Toshihiko Hoashi, Naotaka Serizawa, Kyochika Okabe, Susumu Ichiyama, Rie Shinohara, Yoko Funasaka & Hidehisa Saeki (2017). "Multiple unilaterally localized dermatofibromas in a patient with Down syndrome". The Journal of dermatology. 44 (9): 1074–1076. doi:10.1111/1346-8138.13625. PMID 27665731.
- ↑ J. Stainforth & M. J. Goodfield (1994). "Multiple dermatofibromata developing during pregnancy". Clinical and experimental dermatology. 19 (1): 59–60. PMID 8313640.
- ↑ Yuichiro Tsunemi, Hironobu Ihn, Naoko Hattori, Hidehisa Saeki & Kunihiko Tamaki (2003). "Multiple eruptive dermatofibromas with CD34+ cells in a patient with hypertriglyceridemia". Dermatology (Basel, Switzerland). 207 (3): 319–321. doi:10.1159/000073098. PMID 14571078.
- ↑ H. B. Bargman & I. Fefferman (1986). "Multiple dermatofibromas in a patient with myasthenia gravis treated with prednisone and cyclophosphamide". Journal of the American Academy of Dermatology. 14 (2 Pt 2): 351–352. doi:10.1016/s0190-9622(86)70041-8. PMID 3950136.
- ↑ S. E. Chang, J. H. Choi, K. J. Sung, K. C. Moon & J. K. Koh (2000). "Multiple eruptive dermatofibromas occurring in a patient with acute myeloid leukaemia". The British journal of dermatology. 142 (5): 1062–1063. doi:10.1046/j.1365-2133.2000.03508.x. PMID 10809884.