PCI complications: dissection
|
Percutaneous coronary intervention Microchapters |
|
PCI Complications |
|---|
|
PCI in Specific Patients |
|
PCI in Specific Lesion Types |
|
PCI complications: dissection On the Web |
|
American Roentgen Ray Society Images of PCI complications: dissection |
|
Directions to Hospitals Treating Percutaneous coronary intervention |
|
Risk calculators and risk factors for PCI complications: dissection |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: Cafer Zorkun, M.D., Ph.D. [2], Vanessa Cherniauskas, M.D. [3]
Overview
A coronary artery dissection refers to a split or a tear in the wall of the artery which compresses or compromises the lumen of the artery reducing blood flow. Coronary artery dissection occurs rarely in the absence of percutaneous coronary intervention (PCI). The risk of reduced anterograde flow and lumen narrowing is a relatively (< 3%) uncommon complication of PCI. Significant residual dissections are present in approximately 1.7 % of patients undergoing PCI.[1] Intracoronary stent placement is used to stabilize the dissection.
Classification
The National Heart, Lung and Blood Institute (NHLBI) coronary dissection criteria assign according the severity of coronary dissection following PCI, with the prognostic implications of the coronary dissection depending on extension into the media and adventitia, its axial length, presence of contrast staining, and effect on anterograde coronary perfusion.
Difficulties can be present when assessing the angiographic residual lumen in the presence of coronary dissection due to the frame-to-frame lumen diameter changes using two-dimensional imaging; intravascular ultrasound (IVUS) may be more accurate strategy to provide the true circumference lumen dimensions.
In the NHLBI scheme, dissection is defined as an intraluminal filling defect or flap associated with a hazy, ground-glass appearance. This category is sub-classified using the NHLBI (National Heart Lung and Blood Institute) system for grading dissection types:[2]
Type A
- Type A dissections represent radiolucent areas within the coronary lumen during contrast injection, with minimal or no persistence of contrast after dye has cleared.
Type B
- Type B dissections are parallel tracts or double lumen separated by a radiolucent area during contrast injection, with minimal or no persistence after dye clearance.
Type C
- Type C dissections appear angiographically as contrast outside the coronary lumen ("extraluminal cap") with persistence of contrast in the area after clearance of dye from the coronary lumen.
Type D
- Type D dissections represent spiral ("barber shop pole") luminal filling defects, frequently with extensive contrast staining of the vessel.
Shown below are an animated image and a static image depicting coronary artery dissection type D. Outlined in yellow is the spiral luminal filling defect that characterizes type D coronary artery dissection.
Type E
- Type E dissections appear as new, persistent filling defects.
- As proposed by the Coronary Angioplasty Registry, type E dissection may be caused by thrombus.
Type F
- Type F dissections represent those that lead to total occlusion of the coronary artery, without distal anterograde flow.
- As proposed by the Coronary Angioplasty Registry, type F dissection may be caused by thrombus.
Other Associated Definitions/Terms
- Abrupt closure: Obstruction of contrast flow (TIMI 0 or 1) in a dilated segment with previously documented anterograde flow
- Ectasia: A lesion diameter greater than the reference diameter in one or more areas
- Luminal irregularities: Arterial contour that has a “sawtooth pattern” consisting of opacification but not fulfilling the criteria for dissection or intracoronary thrombus
- Intimal flap: A discrete filling defect in apparent continuity with the arterial wall
- Thrombus: Discrete, mobile angiographic filling defect with or without contrast staining
- Length:Measure end-to-end for type B through F dissections
- Staining: Persistence of contrast within the dissection after washout of contrast from the remaining portion of the vessel
- Perforation Localized: Extravasation of contrast confined to the pericardial space immediately surrounding the artery and not associated with clinical tamponade
- Nonlocalized perforation: Extravasation of contrast with a jet not localized to the pericardial space, potentially associated with clinical tamponade
- Side branch loss: 0, 1, or 2 flow in a side branch > 1.5 mm in diameter which previously had TIMI 3 flow
- Distal embolization: Migration of a filling defect or thrombus to distally occlude the target vessel or one of its branches
- Coronary spasm: Transient or permanent narrowing >50% when a <25% stenosis was previously noted
Pathophysiology
The two primary mechanisms accounting for disruption of the coronary vessel wall include barotrauma and guiding catheter dissections. Most coronary dissections occur as a result of percutaneous coronary intervention, but they may also occur either as an extension of an aortic dissection into the right coronary artery, or in the setting of coronary bypass grafting. Spontaneous coronary artery dissection is itself rare.
Histopathological Findings
-
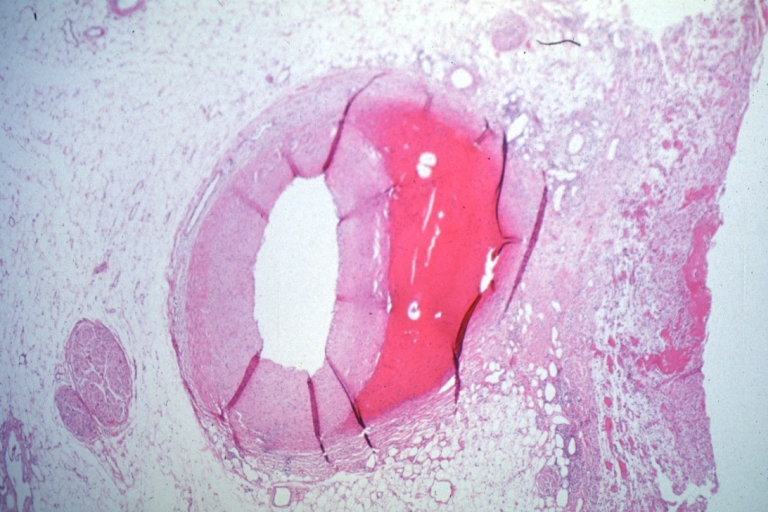
Coronary artery: Dissection Secondary to Trauma: Micro low mag H&E large adventitial hemorrhage this is a diagonal branch of the left anterior descending artery caused massive infarct
-
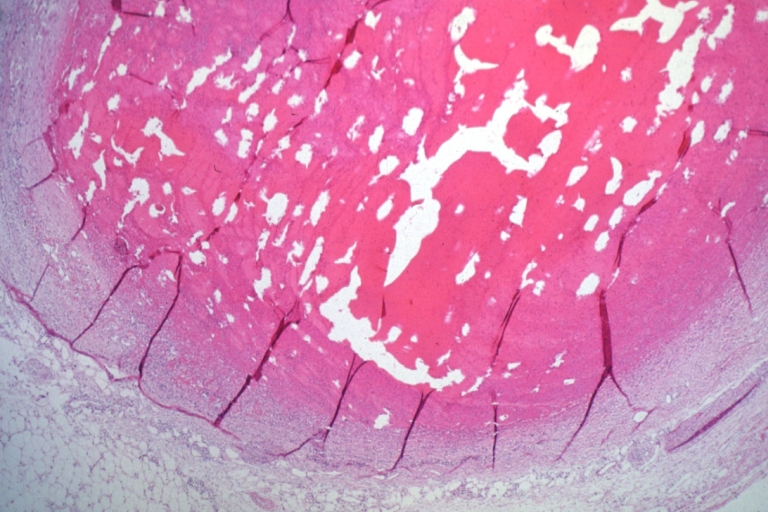
Coronary artery: Dissection Secondary to Trauma: Micro low mag H&E completely occluded LAD
Treatment
Coronary stent placement, surgery and anticoagulation would appear to be reasonable treatment modalities.[3] Given the rare nature of the disease, randomized trial data is obviously lacking. Most intra-procedural dissections can be treated promptly with stenting.
Angiography
Click here to view angiography examples of the different types of coronary artery dissection.
References
- ↑ Laskey WK, Williams DO, Vlachos HA; et al. (2001). "Changes in the practice of percutaneous coronary intervention: a comparison of enrollment waves in the National Heart, Lung, and Blood Institute (NHLBI) Dynamic Registry". Am. J. Cardiol. 87 (8): 964–9, A3–4. PMID 11305987. Unknown parameter
|month=ignored (help) - ↑ Huber, MS.; Mooney, JF.; Madison, J.; Mooney, MR. (1991). "Use of a morphologic classification to predict clinical outcome after dissection from coronary angioplasty". Am J Cardiol. 68 (5): 467–71. PMID 1872273. Unknown parameter
|month=ignored (help) - ↑ Narasimhan, S (2004). "Spontaneous coronary artery dissection (SCAD)" (PDF). IJTCVS. 20 (4): 189–91. doi:10.1007/s12055-004-0084-x.