Mycobacterium avium complex
| Mycobacterium avium subsp. intracellulare | ||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
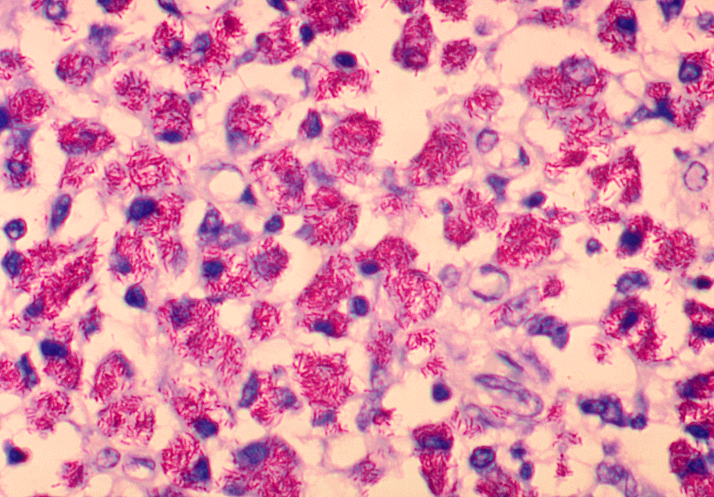 Mycobacterium avium subsp. intracellulare bacteria in lymph tissue.
| ||||||||||||||
| Scientific classification | ||||||||||||||
|
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]
Overview
Mycobacterium avium complex (MAC) is a group of genetically-related bacteria belonging to the genus Mycobacterium. It includes Mycobacterium avium subspecies avium (MAA), Mycobacterium avium subspecies homis (MAH), and Mycobacterium avium subspecies paratuberculosis (MAP).
Historical Perspective
Historically, MAC has also included Mycobacterium avium intracellulare (MAC) – a distinct species of bacteria.
Sources and symptoms
MAC bacteria are common in the environment and cause infection when inhaled or swallowed. Symptoms of MAC diseases are reminiscent of tuberculosis. They include fever, fatigue, and weight loss. Many patients will have anemia and neutropenia if bone marrow is involved. Pulmonary involvement is similar to TB, while diarrhea and abdominal pain are associated with gastrointestinal involvement. MAC should always be considered in a person with HIV infection presenting with diarrhea.
The various subspecies are prevalent in different areas:
- MAA primarily affects birds, but has also been found in the group of mammals known as ruminants, especially deer;
- MAP causes Paratuberculosis, or Johne's Disease;
- MAH is responsible for most MAC diseases in humans, including Hot Tub Lung and Lady Windermere Syndrome. MAC disease is most common in immunocompromised individuals; including senior citizens and those suffering from AIDS or cystic fibrosis.
Mycobacterium avium infection in children
The M. avium and M. haemophilum infection in children form a distinct clinical entity separate from that of AIDS. M. avium typically causes swelling of the lymph nodes of the neck that is usually unilateral. It is not associated with abnormalities of the immune system. The treatment of choice is surgery,[1] with medical treatment (usually clarithromycin and rifabutin for 18 to 24 months) reserved for those patients who cannot have surgery or for whom surgery is not suitable.
MAC in patients with HIV infection
MAC in patients with HIV disease is theorized to represent recent acquisition rather than latent infection reactivating (which is the case in many other opportunistic infections in immunocompromised patients).
The risk of MAC is inversely related to the patient's CD4 count, and increases significantly when the CD4 count decreases below 50 cells/mm³. Other risk factors for acquisition of MAC infection include using an indoor swimming pool, consumption of raw or partially cooked fish or shellfish, bronchoscopy and treatment with granulocyte stimulating factor.
Disseminated disease was previously the common presentation prior to the advent of highly active antiretroviral therapy (HAART). Today, in regions where HAART is the standard of care, localized disease presentation is more likely. This generally includes a focal lymphadenopathy/lymphadenitis.
Diagnosis:
Diagnosis can be achieved through blood cultures, or cultures of other bodily fluids such as lymphatic dranage or stool. Bone marrow culture can often yield an earlier diagnosis, but is usually avoided as an initial diagnostic step because of its invasiveness.
Treatment
Treatment involves a combination of anti-tuberculosis antibiotics. These include:
Antimicrobial Regimen
- 1. Treatment of MAC pulmonary disease [2]
- 1.1. Patients with nodular/bronchiectatic disease
- Preferred regimen: Clarithromycin 1,000 mg three times weekly OR Azithromycin 500–600 mg three times weekly AND Ethambutol 25 mg/kg three times weekly AND Rifampin 600 mg three times weekly
- 1.2. Patients with fibrocavitary or severe nodular/bronchiectatic disease
- Preferred regimen: Clarithromycin 500–1,000 mg/day OR Azithromycin 250–300 mg/day OR Rifampin 600 mg/day OR Rifabutin 150–300 mg/day AND Ethambutol 15 mg/kg/day with consideration of threetimes-weekly Amikacin OR Streptomycin early in therapy
- Note: Patients should be treated until culture negative on therapy for 1 year
- 2. Disseminated MAC disease
- Preferred regimen: Clarithromycin 1,000 mg/day OR Azithromycin 250 mg/day AND Ethambutol 15 mg/kg/day ± Rifabutin 150–350 mg/day
Prophylaxis
- Disseminated MAC disease [3]
- Prophylaxis should be given to adults with acquired immunodeficiency syndrome (AIDS) with CD4+ T-lymphocyte counts less than 50 cells/μl
- Preferred regimen: Azithromycin 1,200 mg/week OR Clarithromycin 1,000 mg/day
- Alternative regimen: Rifabutin 300 mg/day
MAC in immunocompetent patients
Please see information on NTM disease.
References:
Diagnosis and treatment of disease caused by nontuberculous mycobacteria. This official statement of the American Thoracic Society was approved by the Board of Directors, March 1997. Medical Section of the American Lung Association. Am J Respir Crit Care Med 1997; 156:S1.
Teirstein, AS, Damsker, B, Kirschner, PA, et al. Pulmonary infection with MAI: Diagosis, clinical patterns, treatment. Mt Sinai J Med 1990; 57:209.
References
- ↑ Lindeboom JA, Kuijper EJ, van Coppenraet ESB, Lindeboom R, Prins JM (2007). "Surgical excision versus antibiotic treatment for nontuberculous mycobacterial cervicofacial lymphadenitis in children: A multicenter, randomized, controlled trial". Clin Infect Dis. 44: 1057&ndash, 64.
- ↑ Griffith, Daviday E.; Aksamit, Timothy; Brown-Elliott, Barbara A.; Catanzaro, Antonino; Daley, Charles; Gordin, Fred; Holland, Steven M.; Horsburgh, Robert; Huitt, Gwen; Iademarco, Michael F.; Iseman, Michael; Olivier, Kenneth; Ruoss, Stephen; von Reyn, C. Fordham; Wallace, Richarday J.; Winthrop, Kevin; ATS Mycobacterial Diseases Subcommittee; American Thoracic Society; Infectious Disease Society of America (2007-02-15). "An official ATS/IDSA statement: diagnosis, treatment, anday prevention of nontuberculous mycobacterial diseases". American Journal of Respiratory anday Critical Care Medicine. 175 (4): 367–416. doi:10.1164/rccm.200604-571ST. ISSN 1073-449X. Unknown parameter
|pmiday=ignored (help) - ↑ Griffith, David E.; Aksamit, Timothy; Brown-Elliott, Barbara A.; Catanzaro, Antonino; Daley, Charles; Gordin, Fred; Holland, Steven M.; Horsburgh, Robert; Huitt, Gwen; Iademarco, Michael F.; Iseman, Michael; Olivier, Kenneth; Ruoss, Stephen; von Reyn, C. Fordham; Wallace, Richard J.; Winthrop, Kevin; ATS Mycobacterial Diseases Subcommittee; American Thoracic Society; Infectious Disease Society of America (2007-02-15). "An official ATS/IDSA statement: diagnosis, treatment, and prevention of nontuberculous mycobacterial diseases". American Journal of Respiratory and Critical Care Medicine. 175 (4): 367–416. doi:10.1164/rccm.200604-571ST. ISSN 1073-449X. PMID 17277290.
External links
- Mycobacterium avium Complex disease listing information from Center for Disease Control
- MAC fact sheet