Distal radius fracture surgery
|
Distal radius fracture Microchapters |
|
Diagnosis |
|---|
|
Treatment |
|
Case Studies |
|
Distal radius fracture surgery On the Web |
|
American Roentgen Ray Society Images of Distal radius fracture surgery |
|
Risk calculators and risk factors for Distal radius fracture surgery |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1] Associate Editor(s)-in-Chief: Rohan A. Bhimani, M.B.B.S., D.N.B., M.Ch.[2]
Overview
Surgical management of distal radius fracture can present many challenges, particularly in patients with multiple fracture fragments, extensive articular comminution, or metadiaphyseal bone loss. Understanding the column model of distal radius fractures and the goals of reconstruction can be extremely beneficial in preoperative planning and intraoperative decision making. Successful surgical management of complex distal radius fracture requires versatility in surgical approaches and techniques in addition to familiarity with a variety of fixation methods such as volar locking plate, dorsal locking plate, distraction bridge plate and external fixation.
Surgery
- Closed treatment is frequently unsuccessful in maintaining a good position in adults, because there is frequently comminution of the fracture. Re-displacement and deformity can reoccur with an unacceptable ultimate result.
- The radiographic goals for operative fixation of distal radius fractures include:[1][2][3][4]
| Radiological Criteria for Acceptable Reduction of Distal Radius Fracture | ||
|---|---|---|
| Criterion | Normal | Acceptable |
| Ulnar variance (radial length) | ± 2 mm comparing level of lunate facet to ulnar head | No more than 2 mm of shortening relative to ulnar head |
| Radial height | 12 mm | Less than 5 mm |
| Palmar (lateral) tilt | 11 degrees of volar tilt | Neutral |
| Radial inclination | 20 degrees as measured from lunate facet to radial styloid | No less than 10 degrees |
| Intraarticular step or gap | None | Less than 2 mm of either |
Radial Column
- Reconstructing the radial column requires restoring the radial height and inclination and simultaneously obtaining articular congruity with the intermediate column.[5][6]
- If radial shortening is not corrected, the loss of carpal support by the scaphoid facet may transfer loads to the lunate facet, resulting in further articular collapse.
- Failure to correct the loss of radial height may result in decreased grip strength and prohibit maximal clinical outcomes.
- Persistent articular incongruity may also lead to progressive radiocarpal arthrosis.
- Often, a fracture plane will exist between the scaphoid fossa and lunate facet creating an articular step-off (subsidence) or gap (radial translation).
- Failure to address these issues can increase stress on the scapholunate interosseous ligament resulting in attritional attenuation and subsequent ligament insufficiency.
- Since the radial column serves as a buttress to radial translation, stable fixation is necessary to withstand the stresses placed onto it during wrist radioulnar deviation.
Intermediate Column
- Restoration of volar tilt and articular congruity of the lunate facet and sigmoid notch is crucial to successful clinical outcomes.[7][8][9][10]
- Progressive dorsal collapse and radial shortening can lead to an incongruous radiolunate articulation and/or Distal Radio-Ulnar joint (DRUJ) with subsequent instability and arthrosis.
- Additionally, increased ulnar variance can cause painful ulnocarpal impaction syndrome.
- Volar tilt can be maintained by providing stable fixation to the intermediate column with a variety of implants.
- Impacted articular fragments can be elevated and supported with the aid of structural or non-structural bone graft and subchondral fixation.
Pedestal
- Providing a stable foundation to the radial and intermediate columns is the goal of reconstructing the pedestal.
- In the presence of marked metadiaphyseal comminution or bone loss, reinstating the length and bow of the radius, similar to the contralateral forearm, is critical.
Surgical Treatment Options
- A variety of methods and implants exist to stabilize distal radius fractures, ranging from closed reduction and percutaneous pin fixation to the use of intra-medullary devices.
- However, the most common fixation methods to treat complex distal radius fractures include volar locking plates, dorsal plates, fragment-specific implants, external fixation, and distraction bridge plates.
Volar Locking Plate
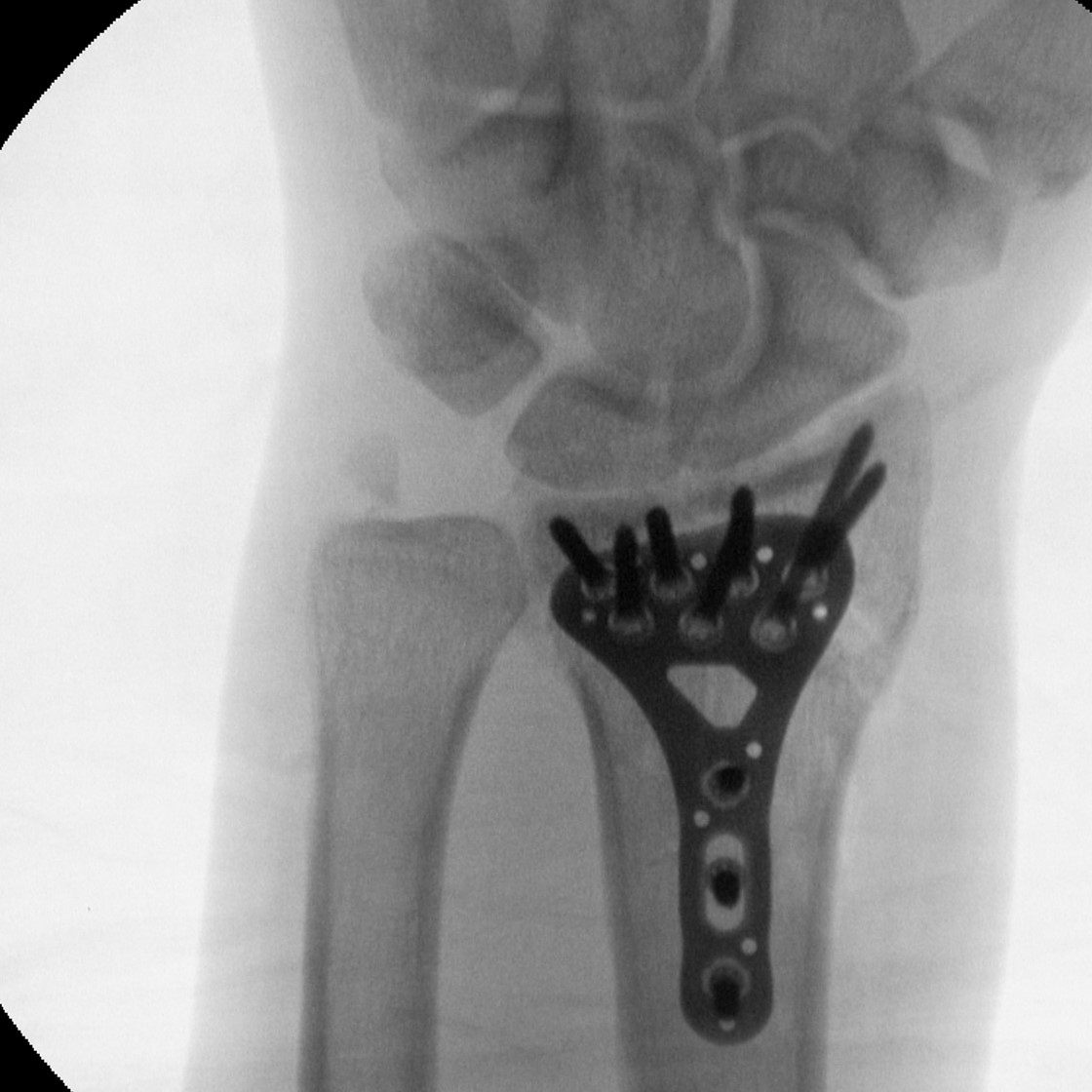 |
The volar locking plate is the mainstay of treatment for intra- and extra-articular distal radius fractures.[11]
- The fixed-angle construct provides stable fixation, even in the setting of metaphyseal comminution, by transferring the forces from the distal fragment to the volar cortex of the intact radial shaft, instead of the dorsal metaphysis.
- The development of variable angle locking screws allows more versatility for plate and screw positioning based on the fracture fragments.
- Volar locking plate fixation can be utilized for management of intra- and/or extra-articular distal radius fractures when the distal fragment is of adequate size for stable screw fixation through the distal row of the locking plate.
Complications of Volar Plating
- Flexor and extensor tendon injuries
- Progressive loss of reduction
- Malreduction
- Intra-articular screw penetration
- Wrist Arhtritis
Dorsal Locking Plate
- Due to the tendency for extension-type distal radius fractures to collapse dorsally, especially in the setting of metaphyseal comminution, a buttress afforded by a dorsal plate can provide excellent stability.[12][13][14]
- In addition, if intra-articular reduction or bone grafting is necessary, the dorsal approach provides outstanding exposure.
- A dorsal plate can be utilized for intra- and/or extra-articular distal radius fractures when adequate dorsal rim/cortex is available for stable screw fixation.
Complications of Dorsal Plating
- Devitalization of the dorsal fragments
- Inadequate purchase due to comminution
- Fracture displacement
- Nerve and extensor tendon irritation
- Wrist arthritis
 |
 |
Fragment Specific Fixation
- Fragment-specific fixation utilizes individualized implants and surgical exposures to reconstruct the various fracture components that form the intermediate and radial columns.[15][16][17]
- Each major fracture component is identified and fixed independently using low profile implants that avoids creating large holes within the small distal fragments.
- These implants create a multi-planar, loadsharing construct that anatomically restores the articular surface while providing enough stability to allow immediate motion after surgery.
- Separate implants can be inserted to stabilize the volar rim, dorsal ulnar corner, dorsal wall, and radial column.
- Fragment-specific fixation has been successfully utilized in the treatment of complex intra-articular distal radius fractures.
Complications of Fragment Specific Fixation
- Implant related soft tissue irritation
- Implant failure
- Neuropraxia of the superficial branch of the radial nerve
External Fixation With or Without Percutaneous Pin Fixation
- Wrist spanning external fixation employs ligamentotaxis to restore and maintain length, alignment, and rotation.[18][19]
- Reduction is typically obtained through closed or minimally open methods and preserves the fracture biology.
- The addition of percutaneous pins enhances the ability to reduce and stabilize fracture fragments.
Complications of External Fixation
- Pin tract infection
- Injury to the superficial branch of the radial nerve
- Complex regional pain syndrome
- Wrist arhtritis
Distraction Bridge Plate
- Distraction bridge plate (DBP) fixation offers an internal method to apply the principles of wrist spanning external fixation to stabilize distal radius fractures.[20][21][22][23]
- Indications:
- Extensive metaphyseal comminution extending proximally into the diaphysis
- Comminuted, intraarticular fractures that are not amenable to standard peri-articular plate fixation
- Concomitant radiocarpal instability
- Unstable distal radius fractures in a polytrauma patient who may benefit from weight bearing through the injured wrist
- Mangled extremities that require extensive soft tissue and bony reconstruction
Complications of Distraction Bridging Plate
- Implant failure
- Malunion
- Nonunion
- Deep infection
- Complex regional pain syndrome
- Extensor tendon injury
Arthroscopic-Assisted Fracture Reduction
- Intra-articular fractures of the radius can be arthroscopically assessed, and reduction of the articular components and assessment and repair of ligamentous injury can then be undertaken.
- Structures at risk include the triangular fibrocartilage complex (TFCC) and the scapholunate ligament.
- TFCC injuries causing obvious DRUJ instability can be addressed at the time of fixation.
Postoperative Rehabilitation
- Complex distal radius fractures warrant individualized immobilization and rehabilitation strategies. For example, forearm rotation may place excessive stress on volar rim with tenuous fixation or on the injured TFCC.
- Similarly, the addition of a thumb spica cast or orthosis with positioning of the wrist in slight ulnar deviation for management of a comminuted radial column fracture may prevent loss of reduction. *Because most multifragmentary distal radius fractures are the result of high-energy injuries, a prolonged period of wrist immobilization and soft-tissue rest may be beneficial and has not been shown to affect clinical outcomes.
- The wrist is typically immobilized for 2 weeks post-operatively in a sugar tong splint with neutral forearm rotation.
- If any instability of the DRUJ was noted intraoperatively, the forearm is splinted in approximately 60 degrees of supination.
- From 2 to 6 weeks post-operatively, the extremity is placed in a short arm or Munster cast based on DRUJ stability.
- At 6 weeks post-operatively, the wrist is placed into a removable orthosis, and active and passive range of motion (ROM) is initiated.
- Full weight bearing commences at approximately 3 months post-operatively after consolidation of the fracture is noted on radiographs.
- The presence of varying degrees of hand, wrist, and elbow stiffness is inevitable and may result from poor pain control, lack of effort in controlled mobilization, edema, concomitant ipsilateral upper extremity fractures, or peripheral nerve injuries.
- Early stretching and mobilization of the intrinsic and extrinsic tendons of the hand is important to prevent finger stiffness.
- Edema control can be initiated with compression gloves, digital massage, and active and passive ROM of the hand.
- A home exercise program or outpatient occupational therapy is started immediately post-operatively to maintain full range of motion of the hand and limit the development of intrinsic muscle tightness.
References
- ↑ Azar, F., Canale, S., Beaty, J. & Campbell, W. (2017). Campbell's operative orthopaedics. Philadelphia, PA: Elsevier. Page: 2990-3007.
- ↑ King HA, Moe JH, Bradford DS, Winter RB (1983). "The selection of fusion levels in thoracic idiopathic scoliosis". J Bone Joint Surg Am. 65 (9): 1302–13. PMID 6654943.
- ↑ Rhee PC, Shin AY (2016). "Management of Complex Distal Radius Fractures: Review of Treatment Principles and Select Surgical Techniques". J Hand Surg Asian Pac Vol. 21 (2): 140–54. doi:10.1142/S2424835516400063. PMID 27454627.
- ↑ Rhee PC, Medoff RJ, Shin AY (2017). "Complex Distal Radius Fractures: An Anatomic Algorithm for Surgical Management". J Am Acad Orthop Surg. 25 (2): 77–88. doi:10.5435/JAAOS-D-15-00525. PMID 28033150.
- ↑ Knirk JL, Jupiter JB (1986). "Intra-articular fractures of the distal end of the radius in young adults". J Bone Joint Surg Am. 68 (5): 647–59. PMID 3722221.
- ↑ Kennedy SA, Hanel DP (2013). "Complex distal radius fractures". Orthop Clin North Am. 44 (1): 81–92. doi:10.1016/j.ocl.2012.08.008. PMID 23174328.
- ↑ Rhee PC, Dennison DG, Kakar S (2012). "Avoiding and treating perioperative complications of distal radius fractures". Hand Clin. 28 (2): 185–98. doi:10.1016/j.hcl.2012.03.004. PMID 22554662.
- ↑ Rozental TD, Blazar PE (2006). "Functional outcome and complications after volar plating for dorsally displaced, unstable fractures of the distal radius". J Hand Surg Am. 31 (3): 359–65. doi:10.1016/j.jhsa.2005.10.010. PMID 16516728.
- ↑ Rozental TD, Beredjiklian PK, Bozentka DJ (2003). "Functional outcome and complications following two types of dorsal plating for unstable fractures of the distal part of the radius". J Bone Joint Surg Am. 85-A (10): 1956–60. PMID 14563804.
- ↑ Orbay JL, Touhami A (2006). "Current concepts in volar fixed-angle fixation of unstable distal radius fractures". Clin Orthop Relat Res. 445: 58–67. doi:10.1097/01.blo.0000205891.96575.0f. PMID 16505728.
- ↑ Schneppendahl J, Windolf J, Kaufmann RA (2012). "Distal radius fractures: current concepts". J Hand Surg Am. 37 (8): 1718–25. doi:10.1016/j.jhsa.2012.06.001. PMID 22763062.
- ↑ Ruch DS, Papadonikolakis A (2006). "Volar versus dorsal plating in the management of intra-articular distal radius fractures". J Hand Surg Am. 31 (1): 9–16. doi:10.1016/j.jhsa.2005.09.011. PMID 16443097.
- ↑ Grewal R, Perey B, Wilmink M, Stothers K (2005). "A randomized prospective study on the treatment of intra-articular distal radius fractures: open reduction and internal fixation with dorsal plating versus mini open reduction, percutaneous fixation, and external fixation". J Hand Surg Am. 30 (4): 764–72. doi:10.1016/j.jhsa.2005.04.019. PMID 16039370.
- ↑ Rein S, Schikore H, Schneiders W, Amlang M, Zwipp H (2007). "Results of dorsal or volar plate fixation of AO type C3 distal radius fractures: a retrospective study". J Hand Surg Am. 32 (7): 954–61. doi:10.1016/j.jhsa.2007.05.008. PMID 17826546.
- ↑ Benson LS, Minihane KP, Stern LD, Eller E, Seshadri R (2006). "The outcome of intra-articular distal radius fractures treated with fragment-specific fixation". J Hand Surg Am. 31 (8): 1333–9. doi:10.1016/j.jhsa.2006.07.004. PMID 17027796.
- ↑ Saw N, Roberts C, Cutbush K, Hodder M, Couzens G, Ross M (2008). "Early experience with the TriMed fragment-specific fracture fixation system in intraarticular distal radius fractures". J Hand Surg Eur Vol. 33 (1): 53–8. doi:10.1177/1753193407087887. PMID 18332021.
- ↑ Gavaskar AS, Muthukumar S, Chowdary N (2012). "Fragment-specific fixation for complex intra-articular fractures of the distal radius: results of a prospective single-centre trial". J Hand Surg Eur Vol. 37 (8): 765–71. doi:10.1177/1753193412439677. PMID 22403437.
- ↑ Grewal R, MacDermid JC, King GJ, Faber KJ (2011). "Open reduction internal fixation versus percutaneous pinning with external fixation of distal radius fractures: a prospective, randomized clinical trial". J Hand Surg Am. 36 (12): 1899–906. doi:10.1016/j.jhsa.2011.09.015. PMID 22051229.
- ↑ Roh YH, Lee BK, Baek JR, Noh JH, Gong HS, Baek GH (2015). "A randomized comparison of volar plate and external fixation for intra-articular distal radius fractures". J Hand Surg Am. 40 (1): 34–41. doi:10.1016/j.jhsa.2014.09.025. PMID 25446409.
- ↑ Hanel DP, Ruhlman SD, Katolik LI, Allan CH (2010). "Complications associated with distraction plate fixation of wrist fractures". Hand Clin. 26 (2): 237–43. doi:10.1016/j.hcl.2010.01.001. PMID 20494750.
- ↑ Richard MJ, Katolik LI, Hanel DP, Wartinbee DA, Ruch DS (2012). "Distraction plating for the treatment of highly comminuted distal radius fractures in elderly patients". J Hand Surg Am. 37 (5): 948–56. doi:10.1016/j.jhsa.2012.02.034. PMID 22480509.
- ↑ Papadonikolakis A, Ruch DS (2005). "Internal distraction plating of distal radius fractures". Tech Hand Up Extrem Surg. 9 (1): 2–6. PMID 16092812.
- ↑ Ruch DS, Ginn TA, Yang CC, Smith BP, Rushing J, Hanel DP (2005). "Use of a distraction plate for distal radial fractures with metaphyseal and diaphyseal comminution". J Bone Joint Surg Am. 87 (5): 945–54. doi:10.2106/JBJS.D.02164. PMID 15866955.