Diagnostic musculoskeletal ultrasound
Editor-In-Chief: Robert G. Schwartz, M.D. [1], Piedmont Physical Medicine and Rehabilitation, P.A.
Overview
Diagnostic Musculoskeletal Ultrasound involves the use of Medical ultrasonography to assess a variety of disorders of the musculoskeletal system. It is far less expensive then MRI,is non invasive, does not involve the use of ionizing radiation and is readily accepted by patients. In physics the term "ultrasound" applies to all acoustic energy with a frequency above human hearing (20,000 hertz or 20 kilohertz). Typical diagnostic sonographic scanners operate in the frequency range of 2 to 18 megahertz, hundreds of times greater than this limit. The choice of frequency is a trade-off between spatial resolution of the image and imaging depth: lower frequencies produce less resolution but image deeper into the body.
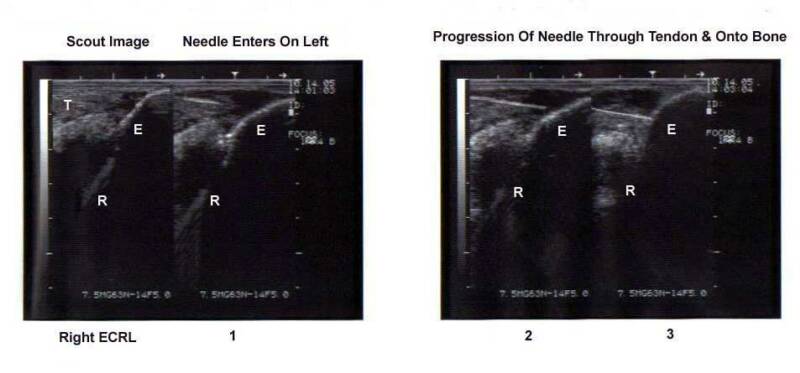
The capability for accurate diagnosis of musculoskeletal conditions has dramatically increased in recent years. In some cases, such as the ability to evaluate motion of tendons and muscles in real-time, it provides valuable information not available from any other modality. In addition, Diagnostic Musculoskeletal Ultrasound has become a valuable guidance tool for procedures such as intra-articular injection, peripheral and spinal nerve block, and percutaneous tenotomy. Disadvantages, such as learning curve, ease of interpretation and image quality have diminished as technology and expertise has increased. Diagnostic Musculoskeletal Ultrasound has become a valuable asset in the diagnostic armamentarium of musculoskeletal injury and pathology.
Diagnostic Applications
Diagnostic Musculoskeletal Ultrasonography is becoming widely used in medicine. It is possible to perform diagnosis or therapeutic procedures with the guidance of ultrasound (for instance percutaneous tenotomy, guided injections, biopsies or drainage of fluid collections). Medical professional sonographers typically use a hand-held probe (called a transducer) that is placed directly on and moved over the patient. A water-based gel is used to couple the ultrasound between the transducer and patient.
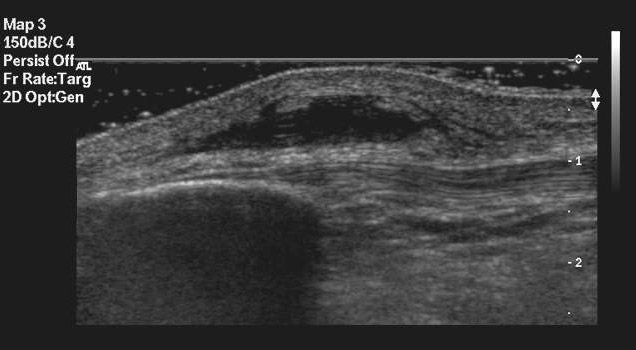
Muscoloskeletal structures such as muscles, tendons, nerve and ligament are imaged at a higher frequencies (7-18 MHz) if they are superficial as these frequencies provide better axial and lateral resolution. Deeper structures are imaged at a lower frequencies (5-10MHz) with lower axial and lateral resolution but greater penetration. Most ultrasound equipment today is capable of imaging over a broad range of frequencies, however specific probes are utilized when different centers of focus (or frequency) are desired.
Medical sonography is used in, for example:
- Ligament injuries
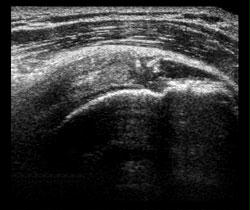
- Tendonopathies and tendonosis
- Muscle injury and atrophy
- Peripheral nerve injury
- Arthropathy
- Cyst and solid mass evaluaiton
- Guidance for injection
- Guidance for percutaneous tenotomy
- Guidance for stem cell and platelet rich plasma (PRP) grafting

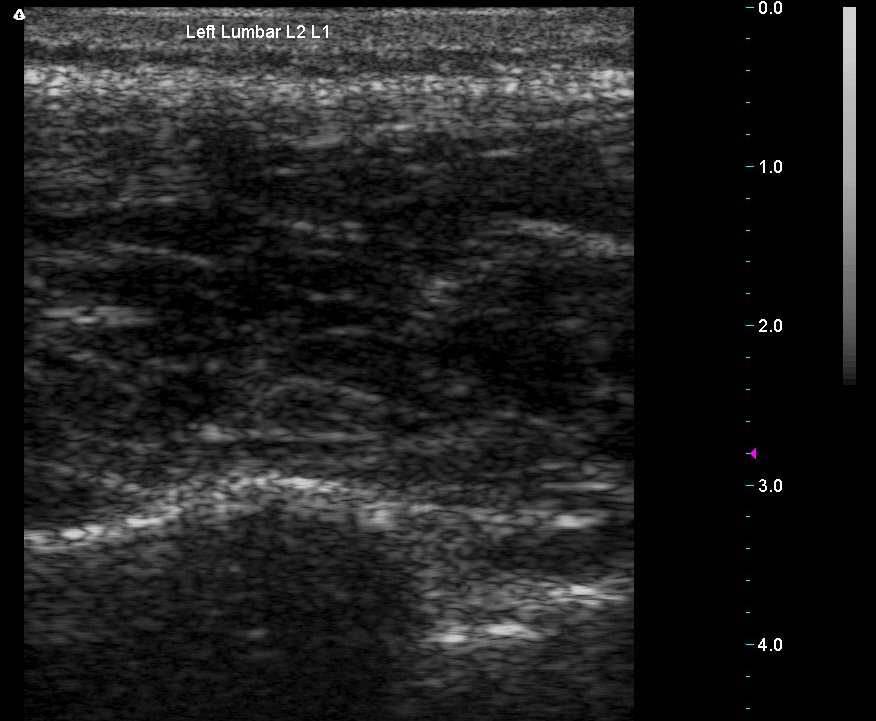
Common areas of study in musculoskeletal ultrasound include the shoulder, wrist and knee, however numerous other applications exist. Virtually any joint, muscle, tendon, ligament or peripheral nerve can be studied. While newer technology for spinal column evaluation with the GE Logiq E9 has been reported, this application has not yet been widely accepted.[1] There are, however numerous references that support the use of musculoskeletal ultrasound for the evalution of paraspinal musculature and interspinous ligament as well as for guidance in spinal injection. At least one peer reviewed blinded study has been published that demonstrated an 85% correlation rate between paraspinal musculoskeletal ultrasound and paraspinal MRI Schwartz, 1999
Strengths of sonography
- It images muscle and soft tissue very well and is particularly useful for delineating the interfaces between solid and fluid-filled spaces.
- It renders "live" images, where the operator can dynamically select the most useful section for diagnosing and documenting changes, often enabling rapid diagnoses.
- It shows the structure of the tissue under study.
- It has no known long-term side effects and rarely causes any discomfort to the patient.
- Equipment is widely available and comparatively flexible.
- Small, easily carried scanners are available; examinations can be performed at the bedside.
- Relatively inexpensive compared to other modes of investigation (e.g. computed X-ray tomography, DEXA or magnetic resonance imaging).
Weaknesses of ultrasonic imaging
- Sonographic devices have trouble penetrating bone.
- Even in the absence of bone or air, the depth penetration of ultrasound is limited, making it difficult to image structures deep in the body, especially in obese patients.
- The method is operator-dependent. A high level of skill and experience is needed to acquire good-quality images and make accurate diagnoses.
Risks and side-effects
Ultrasonography is generally considered a "safe" imaging modality.[2] However slight detrimental effects have been occasionally observed (see below).
Diagnostic ultrasound studies of the fetus are generally considered to be safe during pregnancy. This diagnostic procedure should be performed only when there is a valid medical indication, and the lowest possible ultrasonic exposure setting should be used to gain the necessary diagnostic information under the "as low as reasonably achievable" or ALARA principle.
Studies on the safety of ultrasound
- A study at the Yale Medical School found a correlation between prolonged and frequent use of ultrasound and abnormal neuronal migration in mice.[3]
- A meta-analysis of several ultrasonography studies found no statistically significant harmful effects from ultrasonography, but mentioned that there was a lack of data on long-term substantive outcomes such as neurodevelopment.[4]
References
- ↑ Macios A, "Talk to Me", Radiology Today, 3/23/09;20-23
- ↑ Merritt, CR (Nov 1989). "Ultrasound safety: what are the issues?". Radiology. 173 (2): 304–306. PMID 2678243. Retrieved 2008-01-22.
- ↑ Ang ES Jr, Gluncic V, Duque A, Schafer ME, Rakic P (2006). "Prenatal exposure to ultrasound waves impacts neuronal migration in mice". Proc Natl Acad Sci U S A. 103 (34): 12903–10. PMID 16901978.
- ↑ Bricker L, Garcia J, Henderson J; et al. (2000). "Ultrasound screening in pregnancy: a systematic review of the clinical effectiveness, cost-effectiveness and women's views". Health technology assessment (Winchester, England). 4 (16): i–vi, 1–193. PMID 11070816.
- Musculoskeletal Ultrasound, edited by: Holsbeeck M, Introcaso J, Mosby Year Book, 1991
- Ultrasonography of the Musculoskeletal System, edited by: Montana M, Richardson M. The Radiologic Clinics of North America, vol. 26, no. 1, January 1988
- Schwartz R, Rohan J, Hayden F, "Diagnostic Paraspinal Musculoskeletal Ultrasonography". Journal Of Back And Musculoskeletal Rehabilitation, IOS Press, vol.12, no.1, pg.25-33, 1999
- Guidelines and Gamuts in Musculoskeletal Ultrasound, edited by: Chhem R, Cardinal E, WIley-Liss, 1999
External links
- American Institute of Ultrasound in Medicine Professional Association
- Procedures in Ultrasound (Sonography) for patients, from RadiologyInfo.org
- Ultrasound Safety Issues
- Musculoskeletal Ultrasound Society